
The Cord Blood Donation Process
The cord blood donation process has recently garnered significant attention in the medical field, owing to its life-saving potential and numerous therapeutic applications. This comprehensive guide delves into the intricacies of the cord blood donation process, providing valuable insights and expert analysis to demystify this remarkable medical advancement.
Cord blood, which refers to the blood collected from the umbilical cord and placenta after a baby’s birth, is a rich source of stem cells. These cells possess the unique ability to develop into various cell types, making them a vital component in treating numerous life-threatening diseases and conditions. The cord blood donation process allows for the collection, storage, and eventual utilization of these cells, paving the way for innovative medical treatments and breakthroughs.
Understanding the cord blood donation process is crucial for expectant parents, healthcare professionals, and the general public alike, as it highlights the significance of this resource and its potential to save lives. By exploring the various stages involved in the cord blood donation process, this guide aims to shed light on the procedures, eligibility criteria, and ethical considerations associated with cord blood donation, while also emphasizing its impact on the medical landscape.
Drawing on the expertise of renowned medical professionals, researchers, and industry leaders, this article strives to provide readers with a well-rounded understanding of the cord blood donation process. From the initial stages of pregnancy and prenatal planning, to the cord blood collection methods, and the eventual storage and use of the donated cord blood, this guide offers a comprehensive overview that leaves no stone unturned.
As the cord blood donation process continues to evolve and its applications expand, it is essential for both the public and medical professionals to stay informed on the latest developments, research, and best practices. This guide serves as a reliable source of information and a testament to the tireless efforts of the experts working in the field of cord blood donation and stem cell research.
The cord blood donation process is a vital and rapidly advancing area of medical science that holds immense potential for the future of healthcare. By delving deep into the intricacies of this process, this article aims to educate, inspire, and empower readers to become informed advocates for the life-saving power of cord blood donation.
Significance of Cord Blood Donation
Cord blood donation has emerged as an essential aspect of modern healthcare, offering life-changing therapeutic potential for patients suffering from a wide array of medical conditions. The cord blood donation process, which involves the collection and storage of stem cells found in the umbilical cord blood, has revolutionized the field of regenerative medicine and stem cell research, paving the way for innovative treatments and improved patient outcomes.
One of the key factors that highlight the significance of the cord blood donation process is its unmatched ability to provide a readily available source of stem cells. Unlike other sources of stem cells, such as bone marrow, cord blood can be easily collected and stored without posing any risk to the mother or the newborn child. This non-invasive and low-risk process has made cord blood donation an attractive option for families and healthcare professionals alike.
Moreover, the cord blood donation process has opened new avenues for the treatment of various life-threatening diseases, including leukemia, lymphoma, and certain immune system disorders. The unique properties of cord blood stem cells, such as their ability to rapidly divide and differentiate into a variety of cell types, have made them indispensable in the field of regenerative medicine. As a result, cord blood transplantation has become a viable alternative to traditional bone marrow transplants, offering hope to countless patients worldwide.
Another significant aspect of the cord blood donation process lies in its potential to overcome the limitations associated with donor matching. Cord blood stem cells have been found to be more adaptable when it comes to human leukocyte antigen (HLA) matching, reducing the likelihood of graft rejection and increasing the chances of a successful transplant. This has expanded the pool of potential donors, allowing more patients to benefit from life-saving stem cell therapies.
Furthermore, the cord blood donation process has also played a crucial role in advancing scientific research and knowledge in the field of stem cell biology. The availability of cord blood samples for study has facilitated numerous breakthroughs in our understanding of stem cell behavior, differentiation, and potential applications. This has, in turn, contributed to the development of novel therapies and enhanced our ability to treat previously untreatable conditions.
The significance of the cord blood donation process cannot be overstated. With its unique ability to provide a non-invasive, low-risk source of versatile stem cells, cord blood donation has transformed the landscape of regenerative medicine and stem cell research. By continuing to support and promote the cord blood donation process, we can ensure that more patients benefit from this life-saving resource and drive further advancements in the field of medical science.
Overview of the Donation Process
The cord blood donation process is a carefully designed and regulated procedure that aims to maximize the collection, preservation, and therapeutic potential of cord blood stem cells. This comprehensive overview highlights the critical stages involved in the cord blood donation process, providing a clear understanding of what to expect for expectant parents, healthcare professionals, and potential donors.
The first stage of the cord blood donation process begins with the identification of eligible donors. Prospective donors must meet specific criteria, such as maternal age, overall health, and absence of certain genetic conditions, to ensure the safety and viability of the collected cord blood. It is essential for expectant parents to discuss their interest in cord blood donation with their healthcare provider early in their pregnancy to determine eligibility and make necessary arrangements.
Once eligibility is confirmed, parents must register with a cord blood bank, which could be a public or private institution, depending on their preference and intended use of the cord blood. Public cord blood banks accept donations free of charge, and the donated cord blood is made available for patients in need or research purposes. In contrast, private cord blood banks charge fees for the collection, processing, and storage of cord blood, which is reserved for the donor family’s exclusive use.
The actual cord blood donation process occurs during the delivery of the baby. After the baby is born and the umbilical cord is clamped and cut, the healthcare provider collects the remaining blood from the umbilical cord and placenta using either a gravity bag or a syringe. This collection process is quick, painless, and does not interfere with the birthing experience or pose any risks to the mother or the newborn.
Following the collection, the cord blood is transported to the designated cord blood bank, where it undergoes a series of tests to ensure quality and safety. These tests may include screening for infectious diseases, genetic disorders, and assessing the viability of the stem cells. If the cord blood meets the required standards, it is then processed, cryopreserved, and stored for potential future use.
The cord blood donation process is a seamless and well-orchestrated procedure that provides a valuable source of life-saving stem cells. By understanding the various stages involved in the cord blood donation process, prospective donors can make informed decisions and contribute to the ever-growing pool of cord blood units, ultimately benefiting countless patients in need of stem cell therapies.
Benefits and Potential Applications
The cord blood donation process has garnered significant attention due to its numerous benefits and potential applications in the medical field. By understanding the advantages of cord blood donation and its far-reaching impact, one can appreciate the importance of this life-saving resource and its transformative effect on healthcare.
One of the most notable benefits of the cord blood donation process is its ability to provide a rich source of hematopoietic stem cells (HSCs) that can be used for transplantation. These stem cells possess the unique ability to regenerate blood and immune system cells, making them invaluable in the treatment of various blood disorders, cancers, and immune deficiencies. Unlike other sources of HSCs, such as bone marrow, cord blood can be collected and stored with minimal risk and discomfort to the donor.
Another crucial advantage of the cord blood donation process is the increased likelihood of finding a suitable donor-recipient match. Cord blood stem cells have been found to be more adaptable when it comes to human leukocyte antigen (HLA) matching, reducing the risk of graft rejection and increasing the chances of a successful transplant. This is particularly beneficial for patients from diverse ethnic backgrounds, who often face challenges in finding compatible donors through traditional bone marrow registries.
The cord blood donation process also plays a vital role in advancing research and expanding the potential applications of stem cell therapies. With the increasing availability of cord blood samples, scientists and researchers can explore novel treatment strategies and investigate the underlying mechanisms of stem cell differentiation and regeneration. This has led to breakthroughs in various fields, such as regenerative medicine, where cord blood stem cells have shown promise in treating conditions like spinal cord injuries, heart diseases, and neurological disorders.
Moreover, the cord blood donation process has significant potential in the field of gene therapy, which involves the manipulation of an individual’s genes to treat or prevent disease. Given the unique properties of cord blood stem cells, they could serve as an ideal platform for delivering gene-editing tools, paving the way for personalized medicine and targeted therapies.
The benefits and potential applications of the cord blood donation process are vast and far-reaching. By providing a readily available source of versatile stem cells, cord blood donation has revolutionized the field of transplantation and opened new horizons in regenerative medicine, gene therapy, and stem cell research. As the cord blood donation process continues to evolve and its applications expand, it is essential for both the public and medical professionals to recognize the life-saving potential of this invaluable resource and support its growth and development.
Cord Blood: A Valuable Resource
The medical community has recognized the cord blood donation process as a game-changer due to the numerous advantages it presents over traditional methods of stem cell procurement. Cord blood, which is collected from the umbilical cord and placenta after a baby’s birth, has proven to be a valuable resource with the potential to save lives and advance the field of regenerative medicine.
One of the primary reasons the cord blood donation process is so crucial is the rich source of stem cells it provides. These hematopoietic stem cells possess unique properties, including the ability to self-renew and differentiate into various blood cell types. This makes cord blood an ideal candidate for stem cell transplantation, which is used to treat a wide range of life-threatening diseases, such as leukemia, lymphoma, and certain immune system disorders.
The cord blood donation process has also made stem cell transplantation more accessible to a broader patient population. Since cord blood stem cells require less stringent human leukocyte antigen (HLA) matching compared to bone marrow, the chances of finding a compatible donor are significantly higher. This is particularly beneficial for patients from underrepresented ethnic groups who often struggle to find a suitable match in bone marrow registries.
Another advantage of the cord blood donation process is the ease and safety of collection. Unlike bone marrow donation, which can be invasive and painful, cord blood is collected without any risk or discomfort to the mother or the newborn. This non-invasive process encourages more people to consider cord blood donation, thereby increasing the availability of this valuable resource.
Additionally, the cord blood donation process contributes to the growth of the global cord blood banking industry. Both public and private cord blood banks store cord blood units for future use, either for the donor family or for patients in need. This has led to an increasing number of stored cord blood units worldwide, providing a valuable resource for research, clinical trials, and treatment of various medical conditions.
Cord blood’s value as a resource extends beyond the realm of transplantation. Researchers have been exploring its potential applications in regenerative medicine, where cord blood stem cells show promise in treating a variety of conditions, including neurological disorders, heart diseases, and diabetes. The cord blood donation process plays a crucial role in advancing our understanding of stem cell biology and uncovering novel treatment strategies for previously untreatable conditions.
The cord blood donation process has transformed the landscape of stem cell therapy and regenerative medicine by providing a valuable, easily accessible, and safe resource. Its numerous benefits and potential applications make cord blood an indispensable tool in the ongoing quest to improve patient outcomes and advance medical science.
Definition and Composition
Understanding cord blood and its distinctive composition is crucial as the procedure of cord blood donation becomes more and more significant in the medical world. This knowledge will highlight the importance of the cord blood donation procedure and clarify why it has evolved into a tenet of stem cell therapy and regenerative medicine.
The blood that remains in the placenta and umbilical cord after the delivery of a baby is known as cord blood, as the name suggests. Due to the abundance of hematopoietic stem cells (HSCs) and other crucial biological components in it, it is regarded as a significant resource. These stem cells are essential in the treatment of immune system and blood-related diseases because of their extraordinary capacity to develop into numerous blood cell types, such as red blood cells, white blood cells, and platelets.
These stem cells can be obtained and stored through the process of cord blood donation for potential use in transplantation and research in the future. In comparison to other stem cell sources like bone marrow, the procedure is significantly less intrusive and poses no risk to the mother or the unborn child.
Other crucial biological components, including as mesenchymal stem cells (MSCs), endothelial progenitor cells (EPCs), and different immune cells, can also be found in cord blood in addition to HSCs. Multipotent stem cells, or MSCs, have the capacity to differentiate into many distinct cell types, including bone, cartilage, and fat cells. They also have immunomodulatory characteristics, which may be used to treat autoimmune disorders and raise transplant success rates.
EPCs, on the other hand, are crucial to the angiogenesis process, which is the growth of new blood vessels. It has being investigated whether these cells could be used to treat ischemia illnesses such peripheral artery disease and heart attacks.
Cord blood donation is a vital medical practice because of the distinct characteristics of the blood’s composition. Cord blood contains a variety of stem cells and other biological components that can be used to treat a variety of illnesses and conditions, including immune system problems, tissue repair, and blood malignancies. Additionally, the field of regenerative medicine is constantly developing thanks to the ongoing study on cells produced from cord blood.
The procedure of donating cord blood is crucial in offering a distinct and adaptable supply of stem cells and other biological components. The significance of this procedure and its potential to transform medicine are highlighted by an understanding of its definition and composition. This procedure will provide countless people all over the world hope and a better quality of life.
Unique Characteristics
The cord blood donation process has gained prominence in recent years, primarily due to the unique characteristics of cord blood that set it apart from other sources of stem cells. These distinctive features not only make cord blood an invaluable resource but also contribute to the growing interest and investment in the cord blood donation process.
One of the most significant unique characteristics of cord blood is its rich content of hematopoietic stem cells (HSCs). These stem cells have a remarkable ability to differentiate into various blood cell types, making them an ideal choice for stem cell transplantation to treat blood-related diseases and immune system disorders. This differentiating ability is a key factor driving the cord blood donation process as a valuable alternative to traditional bone marrow transplants.
Another important characteristic of cord blood is its lower requirement for human leukocyte antigen (HLA) matching compared to bone marrow or peripheral blood stem cell sources. This increased compatibility reduces the risk of graft rejection and broadens the pool of potential donors for patients in need of a stem cell transplant. The cord blood donation process is especially beneficial for patients from diverse ethnic backgrounds who often face challenges in finding compatible donors through traditional bone marrow registries.
The cord blood donation process is also unique in its non-invasive and risk-free collection method. Unlike bone marrow or peripheral blood stem cell donations, cord blood is collected from the umbilical cord and placenta after the birth of a baby, without causing any harm or discomfort to the mother or the newborn. This ease and safety of collection make the cord blood donation process an attractive option for expectant parents and healthcare providers alike.
The unique characteristics of cord blood have contributed to the increasing interest and investment in the cord blood donation process. These distinctive features, including the rich content of stem cells, lower HLA matching requirements, and non-invasive collection method, make cord blood an invaluable resource in the field of regenerative medicine and stem cell transplantation.
Therapeutic Potential
The cord blood donation process has opened up new avenues in medical treatments, thanks to the therapeutic potential of cord blood stem cells. These versatile cells have shown great promise in addressing various diseases and conditions, expanding the possibilities for treatment and offering hope to countless patients.
One of the primary therapeutic applications resulting from the cord blood donation process is stem cell transplantation. Cord blood stem cells have been successfully used to treat a wide range of blood-related diseases and immune system disorders, such as leukemia, lymphoma, and sickle cell anemia. The unique properties of cord blood stem cells, including their ability to differentiate into various blood cell types, make them an invaluable resource in treating these conditions.
In addition to their use in stem cell transplantation, cord blood stem cells have demonstrated therapeutic potential in the field of regenerative medicine. Researchers are exploring the possibility of using cord blood stem cells to treat conditions such as heart disease, neurological disorders, and spinal cord injuries. These promising developments are a testament to the importance of the cord blood donation process in advancing medical science.
Furthermore, the cord blood donation process has contributed to the growth of the global cord blood banking industry, which plays a vital role in supporting research and clinical trials. This has resulted in a better understanding of cord blood stem cells and their potential applications, paving the way for the development of innovative treatment strategies and therapies.
The therapeutic potential of cord blood stem cells has positioned the cord blood donation process as a cornerstone in the advancement of medical treatments. As researchers continue to explore new applications and refine existing therapies, the cord blood donation process will continue to play a crucial role in improving patient outcomes and revolutionizing healthcare.
Eligibility for Cord Blood Donation
As the cord blood donation process continues to gain recognition for its numerous benefits and applications, it is essential to understand the eligibility criteria for donating cord blood. By ensuring that donors meet specific requirements, the cord blood donation process can maintain a high-quality supply of cord blood units for transplantation and research purposes.
The first step in determining eligibility for the cord blood donation process is assessing the health of the expectant mother. Generally, a healthy pregnant woman without a history of infectious diseases or certain chronic conditions, such as autoimmune disorders or cancer, can be considered eligible for cord blood donation. It is important to disclose any relevant medical history to the healthcare provider or cord blood bank to ensure the safety and suitability of the donation.
Another crucial factor in the cord blood donation process is the gestational age of the baby. Typically, cord blood donations are only accepted from full-term pregnancies, which are defined as those reaching at least 37 weeks of gestation. This is because the volume of cord blood collected from preterm births may be insufficient for transplantation or research purposes.
In some cases, the eligibility for the cord blood donation process may also depend on the type of delivery. While both vaginal and cesarean deliveries are usually acceptable, certain complications or emergency situations during childbirth might preclude the collection of cord blood. It is essential to discuss your specific circumstances with your healthcare provider to determine whether the cord blood donation process is suitable for you.
Additionally, the cord blood donation process may have specific requirements depending on the cord blood bank or the country in which you reside. Some cord blood banks may have age limits for expectant mothers or specific guidelines regarding the storage and use of donated cord blood. It is crucial to research the requirements and regulations in your area to ensure that you are eligible to participate in the cord blood donation process.
Understanding the eligibility criteria for the cord blood donation process is vital for both expectant parents and healthcare providers. By ensuring that potential donors meet the necessary requirements, the cord blood donation process can maintain a high-quality supply of cord blood units, thereby maximizing the potential benefits and applications of this invaluable resource in the field of regenerative medicine and stem cell transplantation.
Maternal and Neonatal Factors
When considering the cord blood donation process, it is essential to understand the maternal and neonatal factors that can impact the success of the donation. These factors play a crucial role in determining the quality and quantity of cord blood collected, which in turn affects its potential applications in transplantation and research.
One of the primary maternal factors affecting the cord blood donation process is the mother’s health during pregnancy. Conditions such as gestational diabetes, hypertension, or infections can impact the quality of cord blood and may even preclude a woman from donating. It is vital for expectant mothers to maintain a healthy lifestyle and follow their healthcare provider’s recommendations to ensure the best possible outcome for cord blood donation.
In addition to the mother’s health, the neonatal factors, including the baby’s weight and gestational age, can also influence the cord blood donation process. Generally, a higher birth weight is associated with a larger volume of cord blood, which is crucial for successful transplantation and research purposes. As previously mentioned, cord blood donations are typically accepted only from full-term pregnancies (at least 37 weeks of gestation) to ensure a sufficient amount of cord blood is collected.
The timing of cord clamping during childbirth is another factor that can affect the cord blood donation process. Delayed cord clamping, a practice that involves waiting for a few minutes after birth before clamping and cutting the umbilical cord, has been shown to provide various health benefits for the newborn. However, this practice can reduce the volume of cord blood available for collection. Healthcare providers must balance the benefits of delayed cord clamping with the need for adequate cord blood collection, depending on the specific circumstances of each delivery.
Lastly, the method of cord blood collection can also impact the success of the cord blood donation process. Two main methods of cord blood collection are in utero and ex utero. In utero collection takes place immediately after the delivery of the baby but before the delivery of the placenta. In contrast, ex utero collection occurs after the placenta has been delivered. The choice of collection method depends on various factors, including the healthcare provider’s preference and the clinical situation during childbirth.
Understanding the maternal and neonatal factors that impact the cord blood donation process is essential for optimizing the collection and utilization of this valuable resource. By considering these factors and working closely with healthcare providers, expectant parents can make informed decisions about cord blood donation and contribute to the advancement of regenerative medicine and stem cell transplantation.
Health and Safety Guidelines
The cord blood donation process is a vital resource in the field of regenerative medicine and stem cell transplantation, but it is essential to adhere to strict health and safety guidelines to ensure the highest quality of donated cord blood. These guidelines help protect both donors and recipients, maximizing the benefits of the cord blood donation process while minimizing potential risks.
A crucial aspect of the cord blood donation process is the proper screening of expectant mothers. This includes a thorough review of their medical history and the performance of specific tests to rule out infectious diseases or other conditions that could impact the quality of cord blood. It is essential for expectant mothers to disclose any relevant medical information to their healthcare provider or cord blood bank to ensure the safety and suitability of the donation.
During the cord blood donation process, healthcare providers must adhere to aseptic techniques to minimize the risk of contamination. This includes the use of sterile equipment, gloves, and drapes, as well as proper disinfection of the umbilical cord and the surrounding area before collection. By following these strict health and safety guidelines, healthcare providers can significantly reduce the risk of contamination, ensuring that the collected cord blood is suitable for transplantation and research purposes.
The cord blood donation process also requires proper labeling, handling, and transportation of the collected cord blood units. It is crucial to label each unit accurately, including information such as the date and time of collection, maternal and neonatal details, and any other pertinent data. Furthermore, cord blood units should be transported and stored according to specific guidelines, ensuring that the temperature and other storage conditions are maintained to preserve the viability of the stem cells.
Another vital aspect of the cord blood donation process is the ongoing monitoring and accreditation of cord blood banks. These institutions are responsible for the collection, processing, storage, and distribution of donated cord blood units. They must adhere to strict standards and guidelines set forth by regulatory bodies, such as the AABB or FACT, to ensure the quality and safety of the cord blood donation process.
Adhering to strict health and safety guidelines is paramount for the success and credibility of the cord blood donation process. By following these guidelines, healthcare providers, expectant parents, and cord blood banks can work together to ensure the highest quality of donated cord blood, maximizing its potential benefits and applications in the field of regenerative medicine and stem cell transplantation.
Consent and Registration
The cord blood donation process is a critical medical resource that offers hope to countless patients. However, it is essential to ensure that the process is transparent, ethical, and respects the rights of donors. Obtaining proper consent and following the necessary registration procedures are crucial elements in achieving these goals.
Before participating in the cord blood donation process, expectant parents must provide informed consent, demonstrating their understanding of the potential benefits, risks, and implications of donating cord blood. Healthcare providers play a crucial role in educating expectant parents about the cord blood donation process, answering any questions they may have and addressing their concerns. Informed consent ensures that the decision to participate in the cord blood donation process is made voluntarily and without coercion.
In addition to obtaining informed consent, the cord blood donation process requires the completion of specific registration procedures. These procedures vary depending on the cord blood bank or the country in which the donation takes place. Generally, registration involves providing personal and medical information about the expectant mother, the baby’s father (if applicable), and the baby, along with any necessary documentation. This information is crucial for ensuring the safety and suitability of the donated cord blood and for facilitating its eventual use in transplantation or research.
The registration process for the cord blood donation process may also include the selection of a cord blood bank. Expectant parents can choose between public and private cord blood banks, each with its benefits and limitations. Public cord blood banks typically accept donations free of charge and make the donated cord blood available to anyone in need, while private banks store the cord blood exclusively for the family’s use, often at a cost. It is essential for expectant parents to research their options and make an informed decision that aligns with their values and preferences.
Upon successful registration, expectant parents will receive a cord blood collection kit, which will be used by their healthcare provider during the cord blood donation process. It is important to bring this kit to the hospital or birthing center when the time comes for the baby’s delivery.
In conclusion, obtaining informed consent and following the necessary registration procedures are essential elements of the cord blood donation process. By respecting the rights and wishes of expectant parents, healthcare providers and cord blood banks can work together to ensure a transparent and ethical process, maximizing the potential benefits and applications of this invaluable medical resource.
Cord Blood Collection Methods
The success of the cord blood donation process relies heavily on the effectiveness of the cord blood collection methods employed. Two primary methods are used to collect cord blood: in utero and ex utero. Both techniques have their advantages and drawbacks, and the choice between them often depends on the healthcare provider’s preference, the clinical situation during childbirth, and the specific requirements of the cord blood bank.
The in utero method is the most common technique used in the cord blood donation process. It involves collecting cord blood immediately after the baby’s delivery but before the placenta is delivered. The healthcare provider clamps the umbilical cord, then inserts a needle into the umbilical vein and collects the cord blood using a sterile collection bag. The in utero method is generally considered to be the fastest and most efficient technique for collecting cord blood, as it allows for a higher volume of cord blood to be obtained.
In contrast, the ex utero method is employed after the placenta has been delivered. Once the placenta is placed in a sterile container, the healthcare provider punctures the umbilical vein and collects the cord blood, again using a sterile collection bag. Although this method may yield a lower volume of cord blood compared to the in utero technique, it can be a suitable option in certain situations, such as when the delivery is complicated or delayed cord clamping is practiced.
Regardless of the collection method used in the cord blood donation process, it is crucial to adhere to strict health and safety guidelines, as previously mentioned. This includes using sterile equipment, proper disinfection of the umbilical cord, and following aseptic techniques during the collection process. Adhering to these guidelines helps minimize the risk of contamination and ensures the highest quality of donated cord blood.
The choice of cord blood collection method may also depend on the specific requirements of the cord blood bank. Some cord blood banks may have a preference for one method over the other, based on their processing techniques and quality standards. Expectant parents should discuss the available options with their healthcare provider and cord blood bank to determine the most suitable collection method for their situation.
The cord blood donation process depends on effective cord blood collection methods to ensure the best possible outcome. Understanding the advantages and drawbacks of the in utero and ex utero techniques can help healthcare providers and expectant parents make informed decisions about the cord blood donation process, ultimately maximizing the potential benefits and applications of this valuable resource in regenerative medicine and stem cell transplantation.
In Utero vs. Ex Utero Collection
The success of the cord blood donation process relies heavily on the effectiveness of the cord blood collection methods employed. Two primary methods are used to collect cord blood: in utero and ex utero. Both techniques have their advantages and drawbacks, and the choice between them often depends on the healthcare provider’s preference, the clinical situation during childbirth, and the specific requirements of the cord blood bank.
The in utero method is the most common technique used in the cord blood donation process. It involves collecting cord blood immediately after the baby’s delivery but before the placenta is delivered. The healthcare provider clamps the umbilical cord, then inserts a needle into the umbilical vein and collects the cord blood using a sterile collection bag. The in utero method is generally considered to be the fastest and most efficient technique for collecting cord blood, as it allows for a higher volume of cord blood to be obtained.
In contrast, the ex utero method is employed after the placenta has been delivered. Once the placenta is placed in a sterile container, the healthcare provider punctures the umbilical vein and collects the cord blood, again using a sterile collection bag. Although this method may yield a lower volume of cord blood compared to the in utero technique, it can be a suitable option in certain situations, such as when the delivery is complicated or delayed cord clamping is practiced.
Regardless of the collection method used in the cord blood donation process, it is crucial to adhere to strict health and safety guidelines, as previously mentioned. This includes using sterile equipment, proper disinfection of the umbilical cord, and following aseptic techniques during the collection process. Adhering to these guidelines helps minimize the risk of contamination and ensures the highest quality of donated cord blood.
The choice of cord blood collection method may also depend on the specific requirements of the cord blood bank. Some cord blood banks may have a preference for one method over the other, based on their processing techniques and quality standards. Expectant parents should discuss the available options with their healthcare provider and cord blood bank to determine the most suitable collection method for their situation.
The cord blood donation process depends on effective cord blood collection methods to ensure the best possible outcome. Understanding the advantages and drawbacks of the in utero and ex utero techniques can help healthcare providers and expectant parents make informed decisions about the cord blood donation process, ultimately maximizing the potential benefits and applications of this valuable resource in regenerative medicine and stem cell transplantation.
Gravity Bag vs. Syringe Method
In addition to the choice between in utero and ex utero collection methods, healthcare providers also have the option of using different techniques for the actual collection of cord blood during the cord blood donation process. The two primary techniques are the gravity bag method and the syringe method, each with its unique advantages and challenges.
The gravity bag method is a passive technique used in the cord blood donation process, relying on gravity to facilitate the flow of cord blood from the umbilical vein into a sterile collection bag. After clamping the umbilical cord and inserting a needle into the umbilical vein, the healthcare provider allows the cord blood to flow freely into the bag, which is placed below the level of the placenta. This method is relatively simple and requires minimal manipulation by the healthcare provider. However, it can be slower than the syringe method and may result in the collection of a lower volume of cord blood, particularly if the flow of blood from the umbilical cord is slow or obstructed.
On the other hand, the syringe method is an active technique that involves the healthcare provider manually aspirating the cord blood using a sterile syringe. During the cord blood donation process, the healthcare provider inserts a needle into the umbilical vein and carefully draws the cord blood into the syringe. This method allows for greater control over the collection process and can result in a higher volume of cord blood, particularly when the flow from the umbilical cord is slow or obstructed. However, the syringe method requires more skill and experience on the part of the healthcare provider and can be more time-consuming than the gravity bag method.
The choice between the gravity bag and syringe methods during the cord blood donation process often depends on the healthcare provider’s experience, preference, and the specific situation during childbirth. Additionally, cord blood banks may have specific requirements or preferences regarding the collection technique used, based on their processing and quality standards.
Regardless of the technique chosen, it is crucial for healthcare providers to adhere to strict health and safety guidelines during the cord blood donation process, including the use of sterile equipment and aseptic techniques. Ensuring the highest quality of donated cord blood is essential for maximizing its potential benefits and applications in the field of regenerative medicine and stem cell transplantation.
The gravity bag and syringe methods are both viable options for collecting cord blood during the cord blood donation process. Understanding the unique advantages and challenges of each technique can help healthcare providers make informed decisions and optimize the cord blood donation process for the benefit of patients and the advancement of medical research.
Comparison of Efficiency and Safety
When evaluating the cord blood donation process, it is crucial to consider the efficiency and safety of the various collection methods and techniques. Factors such as the volume of cord blood collected, the viability of the stem cells, and the risk of contamination can significantly impact the overall success of the cord blood donation process.
In terms of efficiency, both the in utero and ex utero collection methods can yield sufficient volumes of cord blood for transplantation and research purposes. However, the in utero method is generally considered more efficient, as it often results in a higher volume of cord blood collected. Similarly, the syringe method allows for greater control and can yield a higher volume of cord blood compared to the gravity bag method, particularly in cases where the flow from the umbilical cord is slow or obstructed.
Safety is another critical aspect of the cord blood donation process. Ensuring the highest quality of donated cord blood and minimizing the risk of contamination is essential for the success of cord blood transplantation and research applications. Adherence to strict health and safety guidelines, including the use of sterile equipment and aseptic techniques, is necessary regardless of the chosen collection method or technique.
Comparatively, both the in utero and ex utero methods are considered safe when performed by skilled healthcare providers following the appropriate guidelines. However, the ex utero method may present a slightly higher risk of contamination due to the increased handling of the placenta after delivery. In terms of the gravity bag and syringe methods, the risk of contamination is generally comparable, provided that proper aseptic techniques are followed.
The efficiency and safety of the cord blood donation process depend on the careful selection of collection methods and techniques, as well as the expertise of healthcare providers and adherence to health and safety guidelines. By considering these factors, healthcare providers and expectant parents can optimize the cord blood donation process, ensuring the highest quality of donated cord blood for the benefit of patients and medical research.
Steps in the Cord Blood Donation Process
The cord blood donation process is a vital medical resource that can save lives and advance scientific research. To ensure the success of this process, it is essential to understand and follow the various steps involved in cord blood donation. This comprehensive guide outlines the critical stages in the cord blood donation process.
- Education and Decision-Making: The first step in the cord blood donation process involves educating expectant parents about the potential benefits, risks, and implications of donating cord blood. Healthcare providers play a crucial role in providing information and answering questions, enabling parents to make an informed decision about whether to participate in the cord blood donation process.
- Consent and Registration: If expectant parents decide to proceed with the cord blood donation process, they must provide informed consent and complete the required registration procedures. This typically involves selecting a cord blood bank (public or private) and providing personal and medical information, as well as any necessary documentation.
- Cord Blood Collection Kit: Upon successful registration, expectant parents will receive a cord blood collection kit. This kit contains all the necessary materials and instructions for collecting cord blood during the donation process. It is important to bring this kit to the hospital or birthing center when the time comes for the baby’s delivery.
- Collection Method and Technique: Healthcare providers have several options for cord blood collection during the cord blood donation process. They may choose between in utero and ex utero methods, as well as the gravity bag or syringe techniques. The choice depends on the healthcare provider’s preference, the clinical situation during childbirth, and the requirements of the cord blood bank.
- Cord Blood Collection: The actual cord blood collection occurs during childbirth, immediately after the baby’s delivery. The healthcare provider will clamp the umbilical cord and insert a needle into the umbilical vein to collect the cord blood. The collection process must adhere to strict health and safety guidelines, including the use of sterile equipment and aseptic techniques, to ensure the highest quality of donated cord blood.
- Transportation and Processing: After the cord blood has been collected, it must be transported to the cord blood bank as soon as possible, typically within 48 hours. The cord blood bank will then process the donated cord blood, which involves separating the stem cells from the other blood components, testing for infectious diseases and other potential issues, and preserving the cord blood in a cryogenic storage facility.
- Quality Control and Storage: The cord blood bank will perform various quality control tests throughout the cord blood donation process to ensure the viability and safety of the donated cord blood. Once the cord blood has been processed and deemed suitable for use, it will be stored in a cryogenic facility, ready for potential transplantation or research applications.
- Matching and Transplantation: When a patient requires a stem cell transplant, the cord blood bank will search its inventory for a suitable cord blood unit that matches the patient’s tissue type. If a match is found, the cord blood will be transported to the transplant center, where it will be infused into the patient as part of their stem cell transplantation procedure.
By understanding and following the various steps in the cord blood donation process, healthcare providers and expectant parents can contribute to the success of this vital medical resource. The cord blood donation process has the potential to save lives and advance scientific research, making it a critical aspect of modern regenerative medicine and stem cell transplantation.
Pregnancy and Prenatal Planning
Pregnancy is a critical period for expectant parents to make informed decisions about various aspects of childbirth, including the cord blood donation process. Prenatal planning plays a vital role in ensuring that expectant parents are well-prepared for the potential benefits, risks, and implications of donating cord blood. This section highlights the importance of prenatal planning in the cord blood donation process and provides guidance on how to approach this topic during pregnancy.
- Early Education and Discussion: The first step in prenatal planning for the cord blood donation process is to educate expectant parents about the potential benefits and risks associated with cord blood donation. Healthcare providers should initiate this discussion early in pregnancy, as it allows parents ample time to ask questions, research the topic further, and make an informed decision.
- Choosing a Cord Blood Bank: Once expectant parents have decided to participate in the cord blood donation process, the next step is selecting a cord blood bank. Parents can choose between public cord blood banks, which provide donated cord blood for free to patients in need, and private cord blood banks, which store cord blood for potential future use by the family. This decision should be based on factors such as personal preferences, financial considerations, and the likelihood of needing cord blood for a family member.
- Informed Consent and Registration: After selecting a cord blood bank, expectant parents must provide informed consent and complete the necessary registration procedures. This typically involves filling out forms, providing personal and medical information, and submitting any required documentation. Registration should be completed well before the due date to ensure a smooth cord blood donation process.
- Discussing Collection Methods and Techniques: As part of prenatal planning, healthcare providers should discuss the various cord blood collection methods and techniques with expectant parents. This includes explaining the differences between in utero and ex utero collection, as well as the gravity bag and syringe methods. By understanding these options, parents can make informed decisions and feel more confident about the cord blood donation process.
- Preparing for the Hospital or Birthing Center: It is essential for expectant parents to be well-prepared for the cord blood donation process when they arrive at the hospital or birthing center. This includes bringing the cord blood collection kit and ensuring that the healthcare provider is aware of their intention to donate cord blood. Parents should also discuss any specific requirements or preferences they may have regarding the cord blood donation process with their healthcare provider.
- Post-Delivery Follow-Up: After the birth of the baby and the completion of the cord blood donation process, expectant parents should follow up with their healthcare provider and the cord blood bank. This may include providing additional information, submitting any necessary documentation, and staying informed about the processing and storage of the donated cord blood.
Prenatal planning is a crucial aspect of the cord blood donation process, enabling expectant parents to make informed decisions and prepare for a successful donation experience. By educating parents early in pregnancy, discussing various collection methods and techniques, and guiding them through the registration and preparation process, healthcare providers can help ensure the success of the cord blood donation process, contributing to the advancement of regenerative medicine and stem cell transplantation.
Delivery and Cord Blood Collection
The delivery of a baby is a significant event in the lives of expectant parents, and it is during this time that the cord blood donation process takes place. The collection of cord blood is a critical step, and it is essential for healthcare providers and parents to be well-prepared and informed about this process. This section discusses the key aspects of cord blood collection during delivery and offers guidance on how to ensure a successful donation.
- Timing of Collection: The cord blood donation process takes place immediately after the baby’s delivery. Whether the birth is vaginal or through a cesarean section, the healthcare provider will clamp the umbilical cord and proceed with the cord blood collection. It is crucial to collect the cord blood as soon as possible to maximize the viability of the stem cells and ensure a successful donation.
- Choosing a Collection Method: Healthcare providers have several options for cord blood collection during the cord blood donation process. They may choose between in utero and ex utero methods, as well as the gravity bag or syringe techniques. The choice depends on the healthcare provider’s preference, the clinical situation during childbirth, and the requirements of the cord blood bank.
- Cord Blood Collection Procedure: During the cord blood donation process, the healthcare provider will insert a needle into the umbilical vein and collect the cord blood either in a sterile syringe or a gravity bag. The collection process must adhere to strict health and safety guidelines, including the use of sterile equipment and aseptic techniques, to ensure the highest quality of donated cord blood.
- Handling and Storage: After the cord blood has been collected, it is essential to handle and store it appropriately to maintain its viability. The healthcare provider should gently mix the cord blood with an anticoagulant solution to prevent clotting and place it in a temperature-controlled container or the cord blood collection kit provided by the cord blood bank.
- Transportation and Processing: Following the cord blood donation process, the donated cord blood must be transported to the cord blood bank as soon as possible, typically within 48 hours. The cord blood bank will then process the donated cord blood, which involves separating the stem cells from the other blood components, testing for infectious diseases and other potential issues, and preserving the cord blood in a cryogenic storage facility.
By understanding and following the key aspects of cord blood collection during delivery, healthcare providers and expectant parents can contribute to the success of the cord blood donation process. The collection of cord blood is a vital step in providing life-saving treatments and advancing scientific research, making it essential to approach this process with care and diligence.
vCord Blood Banking and Storage
Once the cord blood has been collected through the cord blood donation process, it is transported to a cord blood bank, where it undergoes processing, testing, and storage. Cord blood banks play a crucial role in preserving this valuable medical resource for future use in stem cell transplantation and research. This section provides an overview of cord blood banking and storage practices, highlighting the importance of maintaining high-quality standards.
- Public vs. Private Cord Blood Banks: Expectant parents have the option to choose between public and private cord blood banks when participating in the cord blood donation process. Public cord blood banks accept donations from the general public, and the donated cord blood is made available to patients in need or for research purposes. Private cord blood banks, on the other hand, store cord blood exclusively for the family that has donated it, usually for a fee.
- Processing of Cord Blood: Upon arrival at the cord blood bank, the donated cord blood undergoes processing to separate the valuable stem cells from other blood components. This involves techniques such as density gradient centrifugation or automated systems that effectively isolate the stem cells while minimizing the risk of contamination.
- Testing and Quality Control: Cord blood banks perform rigorous testing on the donated cord blood to ensure its safety and viability. This includes screening for infectious diseases, such as HIV, hepatitis, and cytomegalovirus, as well as determining the blood type and HLA (human leukocyte antigen) typing. Quality control measures are also in place to assess the viability and potency of the stem cells, ensuring they meet the required standards for transplantation or research use.
- Cryopreservation and Storage: Once the cord blood has been processed and tested, it is preserved using cryopreservation techniques. This involves adding a cryoprotectant agent to the cord blood and gradually cooling it to a temperature of -196 degrees Celsius, where it is stored in liquid nitrogen tanks. This method of storage maintains the integrity and functionality of the stem cells, allowing them to be used for transplantation or research purposes in the future.
- Retrieval and Release: When a patient requires a stem cell transplant, and a suitable cord blood unit is identified, the cord blood bank retrieves the unit from storage and prepares it for shipment to the transplant center. The cord blood bank also provides the necessary documentation and test results to the transplant center to ensure proper matching and safety during the transplantation process.
Cord blood banking and storage practices are essential components of the cord blood donation process, ensuring the availability of high-quality cord blood for patients in need and the advancement of scientific research. By maintaining strict standards for processing, testing, and storage, cord blood banks play a crucial role in the successful application of cord blood in regenerative medicine and stem cell transplantation.
Cord Blood Banking Options
When participating in the cord blood donation process, expectant parents face various options for cord blood banking. These options cater to different preferences, needs, and financial considerations. It is essential for parents to understand the pros and cons of each option to make an informed decision that aligns with their personal values and family circumstances. This section delves into the different cord blood banking options available, providing insights to help guide expectant parents in making the right choice.
- Public Cord Blood Banking: Public cord blood banks collect and store donated cord blood units, making them available for patients in need of a stem cell transplant or for research purposes. The cord blood donation process for public banks is typically free for donors. Public cord blood banks prioritize serving the broader community and contributing to medical research advancements.
Pros:
- No cost to the donor
- Donated cord blood can help save a life or advance medical research
- Supports the wider community by increasing the availability of cord blood units
Cons:
- Donated cord blood is not reserved for the donor’s family
- Limited control over the use of donated cord blood
- Some public banks may have stricter eligibility requirements for donors
- Private Cord Blood Banking: Private cord blood banks store cord blood exclusively for the family that has donated it. These banks charge a fee for their services, which typically includes an initial processing and storage fee, followed by an annual maintenance fee. Families who choose private banking have the assurance that their cord blood unit will be available if needed for a family member.
Pros:
- Cord blood is reserved for the donor’s family, ensuring its availability for future use
- Provides peace of mind for families with a known genetic predisposition to certain diseases
- Greater control over the use and disposition of the cord blood
Cons:
- Can be expensive, with upfront and ongoing fees
- The likelihood of needing the stored cord blood for the family’s use may be low
- Private banks may have varying standards for processing and storage
- Hybrid Cord Blood Banking: Some cord blood banks offer hybrid banking options, which combine aspects of both public and private banking. In this model, a portion of the donated cord blood is stored for the family’s private use, while the remaining portion is made available to the public or for research purposes. This option may appeal to families who want to balance the benefits of both public and private banking.
Pros:
- Offers a balance between the benefits of public and private banking
- Contributes to the greater good while still reserving a portion for family use
- May be more cost-effective than traditional private banking
Cons:
- May still involve significant fees for the private storage portion
- The public portion of the cord blood may not be available to the family if needed
- Limited availability, as not all cord blood banks offer hybrid options
Understanding the various cord blood banking options is a crucial aspect of the cord blood donation process. Expectant parents should weigh the pros and cons of public, private, and hybrid banking, considering factors such as personal preferences, financial constraints, and the likelihood of needing cord blood for a family member. By making an informed decision, parents can ensure the best outcome for their family and contribute to the advancement of cord blood therapy and research.
Public Cord Blood Banks
Public cord blood banks play a vital role in the cord blood donation process by collecting, processing, and storing donated cord blood units for use in stem cell transplantation and medical research. These banks aim to serve the broader community by making cord blood units available to anyone in need, regardless of their ability to pay. This section highlights the features, benefits, and challenges associated with public cord blood banks, providing valuable insights for expectant parents considering this option.
Mission and Goals: Public cord blood banks operate with the mission of increasing the availability of high-quality cord blood units for patients in need of a stem cell transplant. They also support research efforts aimed at advancing the understanding and treatment of various diseases. By participating in the cord blood donation process with a public bank, expectant parents contribute to the greater good and help save lives or advance medical research.
Accessibility and Availability: Public cord blood banks strive to make cord blood units accessible to a diverse range of patients. They aim to increase the inventory of cord blood units from donors of different ethnic backgrounds, improving the chances of finding a suitable match for patients in need. Additionally, public banks often collaborate with international registries to facilitate the sharing of cord blood units across borders, further increasing the availability of life-saving treatments.
Cost and Financial Considerations: Donating cord blood to a public bank is typically free for the donor. The cord blood donation process involves several steps, including collection, processing, and storage, all of which are covered by the public bank. This makes public banking an attractive option for expectant parents who want to contribute to the greater good without incurring additional costs.
Quality Standards and Accreditation: Public cord blood banks adhere to strict quality standards and are accredited by organizations such as AABB, FACT (Foundation for the Accreditation of Cellular Therapy), or the American Society for Blood and Marrow Transplantation (ASBMT). These accreditations ensure that public banks maintain high levels of quality and safety throughout the cord blood donation process, from collection to transplantation.
Challenges and Limitations: Despite the numerous benefits associated with public cord blood banks, they face certain challenges and limitations. For instance, some public banks have stricter eligibility requirements for donors, potentially limiting the number of cord blood units they can collect. Additionally, public banks may struggle with funding and resources, which could affect their ability to maintain and expand their inventory of cord blood units.
Public cord blood banks are a valuable option for expectant parents considering the cord blood donation process. They provide an opportunity to contribute to the greater good by making cord blood units available to patients in need and supporting medical research. By understanding the mission, accessibility, cost considerations, quality standards, and challenges associated with public cord blood banks, parents can make an informed decision that aligns with their values and circumstances.
Benefits and Limitations
When considering the cord blood donation process, it is essential for expectant parents to understand both the benefits and limitations associated with donating cord blood. This section outlines the various advantages and drawbacks of participating in the cord blood donation process, providing a balanced perspective for parents to make an informed decision.
Benefits:
Lifesaving Treatment: Donating cord blood can potentially save lives, as it is a rich source of hematopoietic stem cells that can be used in stem cell transplantation to treat various life-threatening diseases. These include blood cancers like leukemia and lymphoma, as well as genetic disorders such as sickle cell anemia and thalassemia.
Advancement of Medical Research: Cord blood donations contribute to ongoing research efforts aimed at better understanding and developing new treatments for a range of diseases. By participating in the cord blood donation process, expectant parents support the growth of knowledge in the medical field, paving the way for future advancements in stem cell therapy.
Altruistic Contribution: Donating cord blood allows parents to make a meaningful, altruistic contribution to society. By donating cord blood to a public bank, parents help increase the availability of cord blood units for patients in need and provide a potentially life-saving resource for others.
Ease of Collection: The cord blood donation process is straightforward and non-invasive. Cord blood is collected after the birth of the baby, with no risk or discomfort to the mother or newborn. This makes the donation process simple and convenient for parents who choose to participate.
Limitations:
- Limited Control Over Usage: When donating cord blood to a public bank, parents relinquish control over the usage of their donated cord blood unit. This means that the donated cord blood may be used for any patient in need or for research purposes, and the family does not have exclusive access to the cord blood should they require it in the future.
- Storage Constraints: Public cord blood banks are subject to storage constraints, which may result in some cord blood units being discarded if they do not meet the necessary quality standards. This means that not all donated cord blood units will be stored and made available for transplantation or research.
- Eligibility Requirements: The cord blood donation process involves specific eligibility requirements for both the mother and the baby. These requirements may exclude some expectant parents from participating in the cord blood donation process. Factors such as maternal age, health conditions, and a history of infectious diseases can impact eligibility.
- Limited Availability of Public Banks: In some areas, access to public cord blood banks may be limited, which could pose a challenge for parents interested in participating in the cord blood donation process. Limited availability may result in parents needing to arrange for private cord blood banking, which can be expensive.
The cord blood donation process offers various benefits, including the potential to save lives, advance medical research, and provide an altruistic contribution to society. However, parents should also be aware of the limitations, such as limited control over usage, storage constraints, eligibility requirements, and limited availability of public banks. By understanding both the benefits and limitations, expectant parents can make a well-informed decision about whether to participate in the cord blood donation process.
Criteria for Storage
Once expectant parents decide to participate in the cord blood donation process, it is essential to understand the criteria for storing cord blood units. Ensuring that cord blood units meet specific quality standards is crucial for their successful use in stem cell transplantation or medical research. This section discusses the various criteria that cord blood banks consider when deciding whether to store a donated cord blood unit.
Volume of Cord Blood Collected: One of the critical factors in the cord blood donation process is the volume of cord blood collected. An adequate volume of cord blood is necessary to ensure a sufficient number of stem cells for successful transplantation. Generally, public cord blood banks require a minimum volume of 75-100 milliliters of cord blood for storage. If the collected volume falls below this threshold, the cord blood unit may not be stored due to a lower likelihood of successful transplantation.
Cell Viability and Quality: Cord blood banks assess the viability and quality of the hematopoietic stem cells present in the donated cord blood. This includes testing for cell count, cell viability, and sterility. Cord blood units with a high percentage of viable cells and a sufficient number of stem cells are more likely to be stored and used in stem cell transplantation or research.
Maternal and Neonatal Health: Another essential factor in the cord blood donation process is the health of both the mother and the baby. Expectant mothers are required to complete a comprehensive medical and social history questionnaire, which helps cord blood banks identify any potential risks associated with the donated cord blood. Cord blood units from mothers or babies with certain infectious diseases or genetic disorders may not be stored due to the increased risk of complications during transplantation.
Absence of Contamination: Cord blood banks rigorously test donated cord blood units for any signs of contamination, such as bacterial or fungal infections. If a cord blood unit tests positive for contamination, it may not be stored or used for transplantation to ensure the safety of potential recipients.
Accreditation and Regulatory Compliance: Cord blood banks must adhere to strict accreditation and regulatory guidelines to ensure the safety and quality of the cord blood units they store. These guidelines, established by organizations such as AABB and FACT, cover various aspects of the cord blood donation process, including collection, processing, testing, and storage. Compliance with these guidelines helps ensure that stored cord blood units meet the highest quality standards.
Several criteria determine whether a cord blood unit will be stored following the cord blood donation process. Factors such as the volume of cord blood collected, cell viability and quality, maternal and neonatal health, the absence of contamination, and adherence to accreditation and regulatory guidelines all play a role in ensuring the safe and effective storage of cord blood units. By understanding these criteria, expectant parents can better prepare for their participation in the cord blood donation process and contribute to the greater good by providing a valuable resource for patients in need.
Private Cord Blood Banks
While public cord blood banks store donated cord blood units for use by any eligible patient in need, private cord blood banks offer an alternative option for expectant parents considering the cord blood donation process. Private cord blood banks store cord blood units specifically for the donor family’s future use, providing exclusive access to the stored cord blood. This section will discuss the role of private cord blood banks in the cord blood donation process, as well as their advantages and disadvantages.
- Exclusive Access: One of the main reasons families choose private cord blood banking in the cord blood donation process is the assurance of exclusive access to their stored cord blood unit. This means that, should a family member require a stem cell transplant in the future, the stored cord blood unit will be readily available for their use. This can offer peace of mind for parents who have a family history of diseases that may benefit from stem cell transplantation.
- Compatibility: Storing cord blood privately increases the likelihood of a compatible match for family members in need of a stem cell transplant. Cord blood units from a biological relative often have a higher chance of being a suitable match compared to unrelated donors, reducing the risk of transplant-related complications.
- Expanding Treatment Options: As research into cord blood stem cells continues to advance, the range of diseases and conditions treatable with cord blood transplantation may expand. By storing cord blood privately, families may have access to emerging treatments that become available in the future.
However, there are also some disadvantages to private cord blood banking in the cord blood donation process:
- Cost: Private cord blood banking can be expensive, with initial collection and processing fees, as well as ongoing annual storage fees. This financial investment may be a barrier for some families considering private cord blood banking as part of the cord blood donation process.
- Limited Utility: The likelihood of a family member requiring a stem cell transplant is relatively low. Thus, the stored cord blood unit may never be used, and the financial investment in private cord blood banking may not yield any practical benefits.
- Ethical Considerations: Some critics argue that private cord blood banking contributes to health disparities by making potentially life-saving cord blood units available only to those who can afford private storage. This may limit the availability of cord blood units for patients relying on public banks in the cord blood donation process.
Private cord blood banks offer an alternative option for families considering the cord blood donation process. While there are advantages to private cord blood banking, such as exclusive access, compatibility, and expanding treatment options, there are also disadvantages, including cost, limited utility, and ethical considerations. By understanding the role of private cord blood banks in the cord blood donation process, expectant parents can make an informed decision about whether private or public cord blood banking is the best choice for their family.
Benefits and Limitations
The cord blood donation process offers several benefits for both donors and recipients, but there are also some limitations to consider. This section will explore the advantages and disadvantages of the cord blood donation process, helping expectant parents make informed decisions about their participation.
Benefits of the Cord Blood Donation Process:
1. Life-saving Potential: One of the most significant benefits of the cord blood donation process is the potential to save lives. Cord blood stem cells have been successfully used to treat various diseases and conditions, including leukemia, lymphoma, and certain immune disorders. By donating cord blood, expectant parents contribute to a life-saving resource for patients in need of stem cell transplantation.
- Easy and Painless Collection: The cord blood donation process involves the collection of cord blood immediately after the birth of a baby. This procedure is painless for both the mother and the newborn and does not interfere with the bonding process or the delivery routine.
- Lower Graft-versus-Host Disease (GVHD) Risk: Cord blood transplants are associated with a lower risk of GVHD, a potentially severe complication of stem cell transplantation. This is because cord blood stem cells are less mature than those from other sources, such as bone marrow, making them less likely to attack the recipient’s body.
- Increased Genetic Diversity: The cord blood donation process contributes to the diversity of the stem cell donor pool. This is particularly important for patients from ethnic minorities, who may have difficulty finding a compatible match through traditional bone marrow registries.
Limitations of the Cord Blood Donation Process:
- Limited Availability: One of the main limitations of the cord blood donation process is the limited availability of donated cord blood units. Public cord blood banks often have a smaller inventory of units compared to bone marrow registries, making it more challenging for patients to find a compatible match.
- Lower Stem Cell Yield: Cord blood units typically contain fewer stem cells than bone marrow or peripheral blood stem cell donations. This can be a limitation for adult patients or those with larger body masses, who may require a higher number of stem cells for a successful transplant.
- Expiration of Stored Cord Blood: Cord blood units stored in public banks have a limited shelf life, usually around 10-15 years. This means that cord blood units donated today may not be available for use in the future if advancements in medical research increase the demand for stem cell transplantation.
- Eligibility Restrictions: Not all expectant mothers can participate in the cord blood donation process. Various maternal and neonatal factors, such as certain medical conditions, infections, or genetic disorders, may disqualify a potential donor.
The cord blood donation process offers several benefits, including life-saving potential, easy collection, lower GVHD risk, and increased genetic diversity. However, there are also limitations to consider, such as limited availability, lower stem cell yield, expiration of stored cord blood, and eligibility restrictions. By understanding these benefits and limitations, expectant parents can make an informed decision about their participation in the cord blood donation process.
Financial Considerations
The decision to participate in the cord blood donation process is not only a medical and ethical consideration but also a financial one. This section will discuss the financial aspects of the cord blood donation process, including the costs associated with public and private cord blood banking and factors that can influence these expenses.
Public Cord Blood Donation Process:
- Cost-free Donation: One of the primary benefits of the public cord blood donation process is that it is typically free of charge for the donor. Public cord blood banks cover the costs of collection, processing, and storage of the donated cord blood unit, ensuring that financial concerns do not deter potential donors.
- Availability for Patients in Need: When expectant parents choose to donate their cord blood to a public bank, they are contributing to a life-saving resource accessible to patients in need of a stem cell transplant. This altruistic act can make a difference for patients who may not have the financial means to access private cord blood banking services.
Private Cord Blood Banking in the Cord Blood Donation Process:
- Initial Collection and Processing Fees: Families who opt for private cord blood banking in the cord blood donation process should be aware of the initial fees associated with this service. These fees typically cover the costs of cord blood collection, processing, and testing to ensure the cord blood unit is viable for future use. Depending on the chosen private cord blood bank, these fees can range from $1,000 to $3,000.
- Annual Storage Fees: In addition to the initial collection and processing fees, private cord blood banks also charge annual storage fees to maintain the cord blood unit in a cryogenic facility. These fees can range from $100 to $300 per year and must be paid for the entire duration of storage.
- Potential Future Costs: If the privately stored cord blood unit is ever needed for a stem cell transplant, there may be additional costs associated with its release and transportation to the transplant center. These fees can vary depending on the specific circumstances and the policies of the private cord blood bank.
Factors Influencing Cord Blood Banking Costs:
- Geographical Location: The costs associated with the cord blood donation process can vary depending on the geographical location of the donor and the chosen cord blood bank. Some regions may have higher fees due to increased operating costs or limited competition among cord blood banks.
- Special Offers and Discounts: Some private cord blood banks may offer special promotions or discounts to attract customers. Expectant parents considering private cord blood banking should research available offers to potentially reduce the financial burden of the cord blood donation process.
The financial considerations in the cord blood donation process differ between public and private cord blood banking. While public cord blood donation is typically cost-free, private cord blood banking involves initial collection and processing fees, annual storage fees, and potential future costs. By understanding these financial aspects and considering factors that can influence expenses, expectant parents can make an informed decision about their participation in the cord blood donation process.
Ethical Considerations
Apart from the medical, financial, and practical aspects of the cord blood donation process, expectant parents may also face ethical considerations when deciding whether to donate or store their baby’s cord blood. This section will explore some of the ethical issues surrounding the cord blood donation process, including ownership, potential conflicts of interest, and the impact on public health.
Ownership of Cord Blood:
One of the key ethical concerns in the cord blood donation process is the question of ownership. In public cord blood donation, the donated cord blood unit becomes the property of the public bank and is made available to any patient in need of a stem cell transplant. However, in private cord blood banking, the family retains ownership of the cord blood unit, potentially restricting its use to the donor family or a designated recipient.
Potential Conflicts of Interest:
Some critics of the cord blood donation process argue that there may be potential conflicts of interest in the promotion of private cord blood banking. They suggest that some physicians and hospitals may receive financial incentives for promoting private cord blood banking to their patients, potentially leading to biased advice. In response to these concerns, some professional organizations have issued guidelines recommending that healthcare providers disclose any financial ties to cord blood banks and provide balanced information on both public and private cord blood banking options.
Impact on Public Health:
Another ethical consideration in the cord blood donation process is the potential impact on public health. Supporters of public cord blood donation argue that the more cord blood units available in public banks, the higher the chances of finding a suitable match for patients in need of a stem cell transplant. However, when families choose private cord blood banking, the cord blood unit is not available for public use, potentially limiting the availability of life-saving stem cell treatments for patients without access to private cord blood banking.
Equity and Access:
The cord blood donation process also raises ethical questions about equity and access to stem cell treatments. Public cord blood banks provide equal access to donated cord blood units for all patients, regardless of their financial means. In contrast, private cord blood banking is typically only available to families who can afford the associated costs, potentially widening the gap in healthcare access between different socioeconomic groups.
In conclusion, the ethical considerations in the cord blood donation process involve issues of ownership, potential conflicts of interest, the impact on public health, and equity and access to stem cell treatments. By understanding these ethical concerns, expectant parents can make a more informed decision about their participation in the cord blood donation process, weighing the potential benefits and limitations of public and private cord blood banking options.
Informed Consent
Informed consent plays a crucial role in the cord blood donation process, as it ensures that expectant parents understand the potential benefits, risks, and implications of donating or storing their baby’s cord blood. This section will discuss the importance of informed consent, the key components that should be included, and the role of healthcare providers in facilitating informed decision-making for expectant parents.
Importance of Informed Consent:
Informed consent is a fundamental ethical principle in healthcare that ensures patients understand the implications of a medical intervention before they agree to participate. In the context of the cord blood donation process, informed consent ensures that expectant parents have a clear understanding of the procedures involved, the potential benefits and risks, and the differences between public and private cord blood banking options. By obtaining informed consent, healthcare providers can promote autonomy, trust, and transparency in the cord blood donation process.
Key Components of Informed Consent:
For expectant parents to provide informed consent in the cord blood donation process, they should receive clear and comprehensive information about the following aspects:
- Cord blood donation and storage options: Expectant parents should be informed about the differences between public and private cord blood banking, including the potential benefits, limitations, and costs associated with each option.
- Collection process: Information about the cord blood collection process, including the methods used, the associated risks, and the potential impact on the mother and baby, should be provided.
- Testing and storage: Expectant parents should be informed about the testing procedures carried out on cord blood units and the storage conditions in public or private cord blood banks.
- Potential uses of cord blood: Information about the therapeutic potential of cord blood stem cells, including the current and future applications in regenerative medicine and stem cell transplantation, should be provided.
- Risks and limitations: Expectant parents should be informed about the potential risks and limitations of cord blood banking, including the chances of finding a suitable match for transplantation and the potential need for additional stem cell sources.
Role of Healthcare Providers:
Healthcare providers play a pivotal role in ensuring informed consent in the cord blood donation process. They are responsible for providing unbiased and evidence-based information to expectant parents about the cord blood donation process, addressing any questions or concerns, and facilitating informed decision-making. It is essential for healthcare providers to disclose any potential conflicts of interest, such as financial ties to cord blood banks, to ensure transparency and maintain trust in the cord blood donation process.
Informed consent is a vital aspect of the cord blood donation process that ensures expectant parents understand the potential benefits, risks, and implications of donating or storing their baby’s cord blood. Healthcare providers play a critical role in providing clear and comprehensive information, addressing concerns, and facilitating informed decision-making for expectant parents considering the cord blood donation process.
Ownership and Access
When expectant parents decide to participate in the cord blood donation process, they are faced with the choice between public and private cord blood banking. One of the key differences between these options is the matter of ownership and access to the stored cord blood units. This section will explore the implications of ownership and access in the cord blood donation process, discussing the advantages and disadvantages associated with public and private cord blood banking.
Public Cord Blood Banking:
In public cord blood banking, the donated cord blood unit becomes the property of the public bank, which then makes it available for any patient in need of a stem cell transplant. This option promotes the equitable distribution of cord blood units and increases the likelihood of finding a suitable match for patients in need. Public cord blood banks typically operate on a non-profit basis and do not charge families for the collection, processing, and storage of cord blood units.
However, when a family donates cord blood to a public bank, they give up their ownership rights to that unit. As a result, if the donating family later needs a stem cell transplant, they will not have guaranteed access to their previously donated cord blood unit. Instead, they will have to rely on the general availability of suitable matches in the public cord blood bank.
Private Cord Blood Banking:
Private cord blood banking allows families to retain ownership of their baby’s cord blood unit, ensuring that it is reserved exclusively for their use or the use of a designated recipient. This option provides a sense of security for families who may have a higher risk of needing stem cell transplants due to genetic predispositions or family medical history.
However, private cord blood banking comes with significant costs, including initial collection and processing fees as well as ongoing storage fees. Additionally, choosing private cord blood banking may limit the overall availability of cord blood units for patients who rely on public banks to find a match for stem cell transplantation.
Balancing Ownership and Access:
The decision between public and private cord blood banking ultimately depends on the individual needs and priorities of expectant parents. While public cord blood banking promotes equity and access, it requires families to relinquish ownership of their donated cord blood units. In contrast, private cord blood banking guarantees ownership and access but comes with significant costs and may limit the availability of cord blood units for other patients in need.
The ownership and access considerations in the cord blood donation process are important factors for expectant parents to weigh when deciding between public and private cord blood banking. By understanding the advantages and disadvantages of each option, families can make informed decisions that best align with their values, priorities, and financial circumstances.
Privacy and Confidentiality
Privacy and confidentiality are crucial considerations for families participating in the cord blood donation process. Ensuring that sensitive information is protected and that the rights of donors and recipients are respected is essential to maintaining trust in the cord blood banking system. This section will discuss the key aspects of privacy and confidentiality in the cord blood donation process, including the handling of personal information, the use of anonymized data, and the role of regulatory bodies in safeguarding privacy.
Handling of Personal Information:
During the cord blood donation process, personal information, such as medical histories and contact details, is collected from expectant parents. This information is necessary for determining eligibility, coordinating the donation process, and maintaining the quality of stored cord blood units. It is essential that cord blood banks have stringent policies in place to protect the privacy of donors and ensure that personal information is only used for authorized purposes.
Anonymized Data:
To safeguard the privacy of donors and recipients in the cord blood donation process, many cord blood banks employ a system of anonymized data. This means that personal identifiers, such as names and addresses, are removed from cord blood units and replaced with unique identification codes. When a cord blood unit is used for transplantation, the recipient’s healthcare provider will only have access to relevant medical information, such as blood type and human leukocyte antigen (HLA) typing, without being able to identify the donor. This approach maintains the privacy of both parties while still allowing for the effective matching and utilization of cord blood units.
Role of Regulatory Bodies:
Various regulatory bodies oversee the cord blood donation process to ensure that privacy and confidentiality are maintained. In the United States, for example, the Food and Drug Administration (FDA) and the Health Resources and Services Administration (HRSA) play key roles in regulating cord blood banks and establishing guidelines for the protection of privacy. Additionally, organizations such as the AABB (formerly known as the American Association of Blood Banks) and the Foundation for the Accreditation of Cellular Therapy (FACT) provide accreditation and establish standards for the ethical operation of cord blood banks.
These regulatory bodies help ensure that cord blood banks adhere to strict guidelines for the protection of personal information and the maintenance of confidentiality. By following these guidelines, cord blood banks can establish trust with donors and recipients and uphold the integrity of the cord blood donation process.
Privacy and confidentiality are essential components of the cord blood donation process that help maintain trust in the cord blood banking system. By employing robust policies for the handling of personal information, using anonymized data, and adhering to regulatory guidelines, cord blood banks can protect the rights of donors and recipients and ensure that the cord blood donation process remains a valuable and ethical resource for patients in need.
Quality and Safety Standards
The cord blood donation process requires stringent quality and safety standards to ensure the effectiveness of cord blood units and to protect the health of donors and recipients. These standards encompass various aspects of the process, including donor screening, cord blood collection, processing, testing, and storage. This section will discuss the key quality and safety standards in the cord blood donation process and the role of regulatory bodies in enforcing these standards.
Donor Screening:
Before participating in the cord blood donation process, expectant parents must undergo comprehensive donor screening to determine their eligibility. This screening typically includes a review of medical and family history, as well as infectious disease testing. By carefully evaluating potential donors, cord blood banks can minimize the risk of transmitting infections or genetic disorders through cord blood transplantation.
Cord Blood Collection:
The cord blood donation process requires adherence to specific protocols during the collection of cord blood to ensure quality and safety. Collection methods, such as the gravity bag or syringe method, must be carried out by trained professionals following strict aseptic techniques. Proper sterilization of the umbilical cord and appropriate handling of the collected cord blood help reduce the risk of contamination and ensure the viability of the stem cells.
Processing and Testing:
Once collected, cord blood units undergo rigorous processing and testing to ensure quality and safety. Processing involves the separation of stem cells from other blood components and the removal of red blood cells and plasma. This process helps minimize the risk of complications during transplantation. Testing of cord blood units includes determining blood type, HLA typing, and screening for infectious diseases. These tests are essential to ensuring the compatibility of cord blood units with potential recipients and minimizing the risk of adverse reactions.
Storage:
Proper storage of cord blood units is critical to maintaining their quality and safety. Cord blood banks must follow strict protocols for cryopreservation, which involves cooling the cord blood units to extremely low temperatures (-196°C) using liquid nitrogen. This process helps preserve the viability of the stem cells for potential future use. Cord blood banks are also responsible for monitoring storage conditions and maintaining the security and integrity of the stored units.
Role of Regulatory Bodies:
Various regulatory bodies, such as the FDA and HRSA in the United States, oversee the cord blood donation process and enforce quality and safety standards. These bodies develop guidelines and regulations that cord blood banks must follow to ensure the quality and safety of cord blood units. Additionally, accreditation organizations like AABB and FACT establish standards for cord blood banking operations and help promote best practices within the industry.
Quality and safety standards are critical components of the cord blood donation process, ensuring the effectiveness of cord blood units and protecting the health of donors and recipients. By adhering to these standards and following the guidelines set forth by regulatory bodies, cord blood banks can contribute to the ongoing success and credibility of the cord blood donation process.
AABB and FACT Accreditation
Accreditation is an essential aspect of the cord blood donation process, as it ensures that cord blood banks adhere to the highest quality and safety standards. The AABB (formerly known as the American Association of Blood Banks) and FACT (Foundation for the Accreditation of Cellular Therapy) are two prominent organizations that offer accreditation for cord blood banks. This section will discuss the importance of AABB and FACT accreditation in the cord blood donation process and the role these organizations play in maintaining quality and safety standards.
AABB Accreditation:
The AABB is an international, not-for-profit organization dedicated to advancing the practice and standards of transfusion medicine and cellular therapies. AABB accreditation is widely recognized as a symbol of quality and safety in the cord blood banking industry. Cord blood banks seeking AABB accreditation must meet rigorous criteria for donor screening, cord blood collection, processing, testing, storage, and distribution.
The AABB accreditation process involves a thorough assessment of the cord blood bank’s policies, procedures, and facilities. This assessment includes on-site inspections, during which AABB assessors evaluate the cord blood bank’s compliance with established standards. By achieving AABB accreditation, cord blood banks demonstrate their commitment to providing high-quality cord blood units and ensuring the safety of donors and recipients in the cord blood donation process.
FACT Accreditation:
FACT is a non-profit organization that establishes standards for high-quality patient care in the field of cellular therapy. FACT accreditation is a voluntary process that cord blood banks can undergo to demonstrate their adherence to the highest quality and safety standards. Like AABB accreditation, FACT accreditation requires cord blood banks to comply with stringent criteria related to donor screening, cord blood collection, processing, testing, storage, and distribution.
The FACT accreditation process includes a comprehensive review of the cord blood bank’s documentation, policies, and procedures, as well as on-site inspections conducted by FACT inspectors. Achieving FACT accreditation signifies that a cord blood bank has met the rigorous standards for quality and safety set forth by the organization and is dedicated to maintaining these standards throughout the cord blood donation process.
The Importance of AABB and FACT Accreditation:
AABB and FACT accreditation play a crucial role in ensuring the quality and safety of cord blood units in the donation process. By adhering to the standards set forth by these organizations, cord blood banks demonstrate their commitment to providing high-quality cord blood units for transplantation and research. Additionally, these accreditations help to build trust with donors and recipients, as they serve as a reliable indicator of a cord blood bank’s adherence to the highest quality and safety standards.
AABB and FACT accreditation are essential components of the cord blood donation process, as they help ensure that cord blood banks meet the highest standards for quality and safety. By seeking and maintaining accreditation from these organizations, cord blood banks demonstrate their commitment to providing the best possible care for donors and recipients and contribute to the ongoing success of the cord blood donation process.
FDA Regulations
The cord blood donation process is subject to oversight by various regulatory bodies, including the United States Food and Drug Administration (FDA). The FDA plays a crucial role in ensuring the safety and efficacy of cord blood units for transplantation and research purposes. This section will provide an overview of FDA regulations as they pertain to the cord blood donation process, highlighting their importance in maintaining the quality and safety of cord blood products.
The FDA regulates cord blood banks as Human Cell and Tissue-based Products (HCT/Ps) establishments under the Code of Federal Regulations Title 21, Part 1271. These regulations are intended to minimize the risk of transmitting communicable diseases and ensuring the safety of cord blood products for recipients. Some key aspects of FDA regulations in the cord blood donation process include:
- Donor Screening and Testing:
The FDA mandates strict donor screening and testing procedures to minimize the risk of transmitting communicable diseases through cord blood transplantation. Cord blood banks must adhere to FDA guidelines for donor eligibility, which include detailed medical and social history assessments, as well as laboratory testing for infectious diseases such as HIV, hepatitis B and C, and syphilis. - Good Tissue Practice (GTP) Requirements:
FDA regulations require cord blood banks to follow Good Tissue Practice (GTP) requirements, which cover all aspects of the cord blood donation process, including the collection, processing, storage, and distribution of cord blood units. GTP requirements are intended to ensure that cord blood products maintain their integrity, safety, and efficacy throughout the donation process. - Registration and Listing:
Cord blood banks must register with the FDA and provide a list of the HCT/Ps they manufacture. This registration process allows the FDA to maintain oversight of the cord blood banking industry and ensure that establishments comply with applicable regulations. - Reporting Requirements:
The FDA requires cord blood banks to report any adverse events or product deviations that occur during the cord blood donation process. These reporting requirements help the FDA monitor the safety and efficacy of cord blood products and take corrective action when necessary. - Inspections and Compliance:
The FDA conducts inspections of cord blood banks to ensure compliance with regulations governing the cord blood donation process. These inspections may be routine or in response to reported adverse events or product deviations. Failure to comply with FDA regulations can result in enforcement actions, including product recalls, fines, or even the suspension of a cord blood bank’s registration.
The FDA plays a vital role in maintaining the quality and safety of cord blood products through its regulatory oversight of the cord blood donation process. By adhering to FDA regulations, cord blood banks demonstrate their commitment to providing safe and effective cord blood units for transplantation and research purposes. This regulatory framework helps to ensure the ongoing success of the cord blood donation process and safeguards the health and well-being of donors and recipients alike.
Best Practices in Cord Blood Collection
The cord blood donation process plays a crucial role in ensuring the successful collection and preservation of cord blood for future therapeutic use. Implementing best practices in cord blood collection helps maximize the quality and quantity of stem cells obtained, enhancing the chances of successful transplantation. Here are some key considerations and recommended practices for cord blood collection.
- Education and Consent:
Prior to delivery, expectant parents should receive comprehensive education about cord blood donation, including its potential benefits and limitations. Clear and informed consent is essential, ensuring that parents understand the process, their rights, and any associated costs or risks. - Pre-collection Screening:
Screening the expectant mother for infectious diseases, genetic conditions, and other eligibility criteria is crucial to maintain the safety and quality of collected cord blood units. Health questionnaires and medical tests help identify any potential risks or contraindications for donation. - Collection Technique:
Performing the cord blood collection procedure correctly is vital for obtaining an adequate volume of high-quality stem cells. Best practices include:
- Selecting an experienced healthcare professional to conduct the collection.
- Following aseptic techniques to prevent contamination during the procedure.
- Using appropriate anticoagulants and collection bags to ensure the viability of collected cells.
- Timing and Clamping:
The timing of cord clamping is an important consideration. Delaying cord clamping for 30 to 60 seconds after birth allows for an optimal volume of blood to be collected. This practice enhances the number of stem cells obtained, as more blood transfers from the placenta to the baby. - Transportation and Processing:
Efficient transportation and timely processing of cord blood samples are critical for preserving cell viability. Using validated transportation containers and ensuring prompt delivery to the processing facility help maintain the quality of the collected cord blood. Processing should occur within a specified time frame to prevent cell degradation. - Quality Control and Testing:
Stringent quality control measures should be in place throughout the cord blood donation process. This includes testing for infectious diseases, blood type confirmation, and evaluating the total nucleated cell count and viability of collected cells. These measures ensure that the cord blood unit meets the required standards for transplantation. - Donor Privacy and Confidentiality:
Maintaining donor privacy and confidentiality is crucial throughout the cord blood donation process. Personal information should be handled securely and protected in compliance with relevant privacy regulations. - Donor Follow-up:
Regular communication and follow-up with donors can help ensure ongoing donor satisfaction and engagement. Providing updates on the status of the donated cord blood unit and its potential impact on patients in need can foster a sense of fulfillment and support for the donation process.
Implementing these best practices in cord blood collection can enhance the quality and viability of donated cord blood units. Continuous evaluation and improvement of the donation process, along with adherence to regulatory guidelines, contribute to the overall success of cord blood banking and its potential for therapeutic applications.
Cord Blood Transplantation
The cord blood donation process has significantly contributed to the advancement of cord blood transplantation, a potentially life-saving procedure for patients with various blood disorders, immune deficiencies, and certain types of cancers. This section will explore how the cord blood donation process plays a critical role in facilitating successful cord blood transplantations and discuss the benefits of this procedure for patients in need.
One of the main advantages of the cord blood donation process is the increased availability of cord blood units for transplantation. As more people become aware of the benefits of cord blood donation and opt to participate, the number of stored cord blood units continues to grow. This expansion of the cord blood inventory has made it easier for patients to find suitable matches, particularly for those from diverse ethnic backgrounds who may have difficulty finding a compatible donor through traditional bone marrow registries.
Moreover, the cord blood donation process has led to advancements in cord blood transplantation techniques. As more cord blood units become available for research and clinical use, scientists and clinicians can refine their understanding of cord blood stem cells and develop more effective transplantation strategies. For example, the cord blood donation process has contributed to the development of novel approaches such as double cord blood transplantation, which involves transplanting stem cells from two different cord blood units to increase the chances of engraftment and improve patient outcomes.
The cord blood donation process also plays a vital role in maintaining the quality and safety of cord blood units for transplantation. By adhering to strict guidelines and regulatory requirements, cord blood banks ensure that cord blood units are free from infectious agents and possess the necessary cellular content for successful transplantation. The rigorous screening, testing, and processing methods implemented throughout the cord blood donation process help to optimize the efficacy of cord blood transplantations and minimize potential risks for patients.
Cord blood transplantation offers several advantages over traditional bone marrow transplantation. Cord blood units can be readily available for transplantation, reducing the time patients have to wait for a suitable donor. Furthermore, the chances of graft-versus-host disease (GVHD), a potentially severe complication of stem cell transplantation, are generally lower with cord blood transplants compared to bone marrow transplants. This reduced risk is primarily due to the immature immune cells present in cord blood, which are less likely to attack the recipient’s tissues.
The cord blood donation process has greatly impacted the field of cord blood transplantation by increasing the availability of cord blood units, advancing transplantation techniques, and ensuring the quality and safety of cord blood products. As a result, cord blood transplantation has become a valuable treatment option for many patients with life-threatening diseases, offering them hope for a better future.
Indications and Success Rates
The cord blood donation process has been a game-changer for patients with various life-threatening diseases who require stem cell transplants. As more people participate in cord blood donation, researchers and clinicians gain a deeper understanding of the indications for cord blood transplantation and its success rates. This section will discuss the conditions for which cord blood transplantation is indicated and the success rates associated with this innovative treatment modality.
The cord blood donation process has facilitated the use of cord blood transplantation in treating a wide range of diseases. Some of the primary indications for cord blood transplantation include hematological malignancies such as leukemia, lymphoma, and myelodysplastic syndromes. The cord blood donation process also enables transplantation for patients with non-malignant disorders, including aplastic anemia, sickle cell anemia, thalassemia, and certain inherited immune deficiencies.
One of the critical aspects of the cord blood donation process is the ability to provide a diverse pool of potential donors, increasing the likelihood of finding a suitable match for patients who may not have a compatible donor within their family or the bone marrow registries. This is particularly important for patients from ethnic minority populations, who often face challenges in finding a matched donor due to the underrepresentation of their ethnic groups in the registries.
The success rates of cord blood transplantation are influenced by several factors, including the quality and quantity of stem cells obtained through the cord blood donation process. High-quality cord blood units, which are rich in stem cells and free from contamination, have a better chance of leading to successful engraftment and improved patient outcomes. The cord blood donation process adheres to strict guidelines and regulatory standards to ensure that cord blood units meet these quality criteria.
Additionally, the success rates of cord blood transplantation are affected by the degree of human leukocyte antigen (HLA) matching between the donor and recipient. The cord blood donation process has made it possible to identify and store a diverse array of HLA types, increasing the chances of finding a well-matched donor for patients in need. While cord blood transplantation has a higher degree of HLA mismatch tolerance compared to bone marrow transplants, a better HLA match generally translates to a higher probability of transplant success and lower risk of complications such as graft-versus-host disease.
The cord blood donation process has been instrumental in expanding the indications for cord blood transplantation and providing insights into its success rates. By increasing the availability of high-quality cord blood units and fostering a diverse pool of potential donors, the cord blood donation process has made it possible for countless patients to benefit from life-saving stem cell transplants.
HLA Matching and Donor Selection
The cord blood donation process plays a crucial role in ensuring the availability of stem cell sources for transplantation. One of the most critical aspects of this process is human leukocyte antigen (HLA) matching and donor selection. In this section, we will discuss the importance of HLA matching in the cord blood donation process and how it impacts donor selection and transplant outcomes.
HLA matching is essential in the cord blood donation process because it determines the compatibility between the donor’s stem cells and the recipient’s immune system. A closer match between the donor and recipient helps minimize the risk of transplant-related complications, such as graft-versus-host disease (GVHD) and graft rejection. The cord blood donation process involves testing and analyzing the HLA profile of donated cord blood units to find the most suitable match for patients requiring transplantation.
The cord blood donation process has several advantages in terms of HLA matching and donor selection compared to traditional bone marrow or peripheral blood stem cell transplants. Due to the unique immunological properties of cord blood stem cells, cord blood transplants can tolerate a higher degree of HLA mismatch. This flexibility in HLA matching makes the cord blood donation process particularly valuable for patients who cannot find a closely matched donor within their family or the bone marrow registries.
In the cord blood donation process, donor selection involves considering several factors in addition to HLA matching. Some of these factors include the quality and quantity of the donated cord blood, the donor’s age, and the absence of infectious diseases. The cord blood donation process follows strict guidelines to ensure that only the highest quality cord blood units are selected and stored for future transplantation.
One of the challenges in the cord blood donation process is the limited volume of stem cells typically found in cord blood units. This constraint can impact the success of transplantation, particularly for adult patients or those with larger body masses. To address this issue, the cord blood donation process often involves combining multiple cord blood units or using other stem cell sources to supplement the cord blood transplant, depending on the patient’s needs.
HLA matching and donor selection are vital components of the cord blood donation process. Ensuring a suitable match between the donor and recipient is key to maximizing the chances of a successful transplant and minimizing potential complications. The cord blood donation process has opened new avenues for patients who cannot find a compatible donor through traditional methods, offering hope for those in need of life-saving stem cell transplants.
Transplant Process and Potential Complications
The cord blood donation process serves as a vital source of stem cells for patients in need of a transplant. As with any medical procedure, the transplant process involving cord blood stem cells carries some risks and potential complications. In this section, we will discuss the steps involved in the cord blood transplant process and address some of the potential complications that may arise.
The cord blood donation process begins with the collection and storage of cord blood units, followed by HLA matching and donor selection, as discussed in previous sections. Once a suitable cord blood unit is identified, the transplant process can commence. The cord blood transplant process generally involves the following steps:
- Preparatory Regimen: The recipient undergoes a conditioning regimen, which typically includes chemotherapy and/or radiation therapy. This step aims to eliminate the patient’s diseased or damaged cells and suppress their immune system to reduce the risk of graft rejection.
- Stem Cell Infusion: The donated cord blood unit is thawed and infused into the patient’s bloodstream, where the stem cells travel to the bone marrow and begin producing new blood cells.
- Engraftment: This phase of the cord blood transplant process involves the successful integration of the donor’s stem cells into the recipient’s bone marrow, leading to the production of healthy blood cells.
- Recovery and Follow-up: After engraftment, the patient is closely monitored for any signs of complications or infections. The recovery period varies depending on the patient’s condition and response to the transplant.
The cord blood donation process, like any other transplant procedure, carries some inherent risks and potential complications. Some of the most common complications associated with the cord blood transplant process include:
- Graft-versus-host disease (GVHD): This complication occurs when the donor’s immune cells attack the recipient’s body, leading to symptoms ranging from mild to life-threatening. The unique properties of cord blood stem cells make them less likely to cause GVHD compared to other stem cell sources.
- Graft rejection: The recipient’s immune system may recognize the donor cells as foreign and attempt to destroy them, resulting in graft rejection. The risk of rejection is generally lower in cord blood transplants due to the greater tolerance for HLA mismatches.
- Infections: Patients undergoing the cord blood transplant process are at an increased risk of infections due to their weakened immune systems during the preparatory regimen and recovery phase.
- Delayed engraftment: Cord blood transplants may take longer to engraft compared to other stem cell sources, potentially increasing the risk of complications.
Despite these potential complications, the cord blood donation process has proven to be a valuable and life-saving resource for many patients. The unique properties of cord blood stem cells, combined with the increased availability of cord blood units through public and private banks, have expanded the potential for successful stem cell transplants for patients with various medical conditions.
The cord blood donation process offers a promising source of stem cells for transplantation. While there are inherent risks and potential complications, the benefits of cord blood transplants often outweigh the risks for many patients in need of a life-saving transplant.
Current Research and Future Potential
The cord blood donation process has already proven to be a crucial resource in the field of regenerative medicine. With the unique properties of cord blood stem cells, researchers are continuously exploring new applications and possibilities for the future. In this section, we will discuss the current state of research and the potential future developments in the cord blood donation process.
Currently, the cord blood donation process is primarily utilized for hematopoietic stem cell transplantation (HSCT) in the treatment of various blood-related disorders and cancers. Cord blood has become an increasingly popular alternative to bone marrow and peripheral blood stem cell transplants, due to its unique advantages such as lower risk of graft-versus-host disease (GVHD) and a higher tolerance for human leukocyte antigen (HLA) mismatches.
Beyond its established applications, the cord blood donation process has the potential to play a significant role in future medical advancements. Researchers are investigating the use of cord blood stem cells in several innovative areas, including:
- Regenerative Medicine: The potential of cord blood stem cells to differentiate into various cell types has spurred interest in their use for tissue repair and regeneration. For example, researchers are exploring the use of cord blood stem cells in the treatment of heart disease, diabetes, and neurodegenerative disorders such as Parkinson’s and Alzheimer’s.
- Immunotherapy: Cord blood stem cells have unique immunomodulatory properties that could be harnessed for therapeutic purposes. Current research is focusing on utilizing cord blood stem cells for the development of novel immunotherapies to treat autoimmune diseases, inflammatory conditions, and certain types of cancer.
- Gene Therapy: The cord blood donation process could potentially contribute to the rapidly evolving field of gene therapy. Scientists are investigating the possibility of using cord blood stem cells as a vehicle for delivering functional genes to patients with genetic disorders, thereby offering a potential cure for conditions like sickle cell anemia, thalassemia, and severe combined immunodeficiency (SCID).
As research in these areas progresses, the cord blood donation process will likely become even more valuable in the future. The expansion of cord blood banking options, coupled with ongoing research, could significantly increase the availability of cord blood units for patients in need of life-saving treatments.
Moreover, as our understanding of cord blood stem cells advances, we may also develop more efficient methods for collecting, processing, and storing cord blood units. This could lead to improved success rates in transplantation and a broader range of therapeutic applications for cord blood stem cells.
The cord blood donation process has already made a significant impact in the field of regenerative medicine and transplantation, but the future holds even greater potential. With ongoing research and advancements, the cord blood donation process is poised to play an essential role in shaping the future of medical treatments for a variety of disorders and conditions.
Regenerative Medicine
The field of regenerative medicine has gained significant momentum in recent years, offering hope for the treatment of various diseases and conditions. One of the most promising resources in this area is the cord blood donation process, which provides access to a rich source of stem cells that can be harnessed for regenerative purposes. In this section, we will delve into how the cord blood donation process is contributing to advancements in regenerative medicine and its potential applications.
Cord blood, obtained through the cord blood donation process, is a rich source of hematopoietic stem cells (HSCs) and mesenchymal stromal cells (MSCs), which have the unique ability to differentiate into various cell types. This characteristic makes them highly valuable for regenerative medicine, as they can be used to replace damaged or diseased tissue, potentially restoring normal function in patients.
Some of the key areas where the cord blood donation process is contributing to the development of regenerative medicine include:
- Cardiovascular Disease: Researchers are exploring the potential of cord blood stem cells to repair damaged heart tissue following a heart attack. Preclinical studies have shown promising results, with cord blood stem cells promoting the growth of new blood vessels and improving cardiac function.
- Neurological Disorders: The cord blood donation process may play a crucial role in developing treatments for neurodegenerative diseases such as Alzheimer’s and Parkinson’s. Cord blood stem cells have been found to secrete neurotrophic factors that promote neuronal survival and reduce inflammation in the brain, providing a potential therapeutic avenue for these devastating conditions.
- Diabetes: The cord blood donation process may also offer hope for patients with Type 1 diabetes. Researchers are investigating the use of cord blood stem cells to regenerate insulin-producing beta cells in the pancreas, which could potentially lead to a cure for this chronic disease.
- Orthopedic Applications: The cord blood donation process may contribute to the development of novel treatments for various orthopedic conditions, such as osteoarthritis and bone fractures. Mesenchymal stromal cells derived from cord blood have demonstrated the ability to differentiate into bone, cartilage, and other connective tissues, making them a promising resource for tissue repair and regeneration.
As research in these areas continues to progress, it is essential to recognize the importance of the cord blood donation process in providing the necessary resources for these groundbreaking therapies. With the growing demand for cord blood stem cells, public and private cord blood banks play a critical role in ensuring the availability of this valuable resource.
The cord blood donation process is a vital component in the advancement of regenerative medicine, providing researchers with access to unique stem cells with enormous therapeutic potential. By continuing to support and promote the cord blood donation process, we can help unlock the full potential of regenerative medicine, offering new hope for patients suffering from a wide range of diseases and conditions.
Gene Therapy
Gene therapy is an emerging field of medicine that aims to treat or prevent diseases by directly targeting and modifying the genetic material within a patient’s cells. The cord blood donation process has emerged as a valuable source of stem cells, which can be employed in gene therapy techniques to potentially treat a variety of genetic disorders and other conditions. In this section, we will explore how the cord blood donation process is contributing to the advancement of gene therapy and its potential applications.
The cord blood donation process involves collecting and storing the blood remaining in the umbilical cord and placenta after childbirth, which is rich in hematopoietic stem cells (HSCs). These HSCs can give rise to all types of blood cells, making them an attractive target for gene therapy approaches aimed at correcting blood-related genetic disorders.
One of the key advantages of using cord blood stem cells in gene therapy is their ability to self-renew and differentiate into various cell types. This property allows scientists to genetically modify cord blood stem cells outside the body and then reintroduce them into the patient, where they can engraft, multiply, and produce healthy blood cells with the corrected gene.
Some of the main areas where the cord blood donation process is supporting the development of gene therapy include:
Inherited Blood Disorders: The cord blood donation process has played a critical role in the development of gene therapies for inherited blood disorders such as sickle cell disease and thalassemia. By modifying the genetic material within cord blood stem cells, researchers can correct the underlying genetic defect and potentially cure the disease.
Immunodeficiencies: Gene therapy using cord blood stem cells from the cord blood donation process is also being investigated as a potential treatment for severe combined immunodeficiency (SCID) and other inherited immune system disorders. By correcting the faulty gene responsible for these conditions, gene therapy could restore normal immune system function and protect patients from life-threatening infections.
Cancer: The cord blood donation process may contribute to the development of innovative gene therapy approaches for cancer treatment. One promising strategy involves genetically engineering cord blood stem cells to produce immune cells that can specifically target and destroy cancer cells.
Metabolic Disorders: The cord blood donation process could also support gene therapy research for metabolic disorders such as lysosomal storage diseases. By introducing a functional copy of the missing or faulty gene into cord blood stem cells, it may be possible to restore normal enzyme function and alleviate symptoms of these debilitating conditions.
The cord blood donation process is a valuable resource for the advancement of gene therapy, offering a unique source of stem cells with significant therapeutic potential. As research in this area continues to evolve, the cord blood donation process will play a critical role in providing the necessary resources to develop new and effective treatments for various genetic disorders and other conditions.
Expansion of Therapeutic Applications
The cord blood donation process is rapidly advancing as a pivotal tool in modern medicine, providing a rich source of hematopoietic stem cells (HSCs) for various therapeutic applications. As scientists continue to delve into the potential of cord blood stem cells, the scope of treatable conditions is expanding, pushing the boundaries of regenerative medicine and offering hope to patients with previously untreatable diseases. This section highlights the expansion of therapeutic applications resulting from the cord blood donation process and explores the exciting possibilities that lie ahead.
The cord blood donation process has already demonstrated its utility in treating over 80 blood-related disorders, including leukemia, lymphoma, and various inherited blood diseases. However, ongoing research is revealing new applications for cord blood stem cells in areas beyond blood disorders:
- Neurological Disorders: The cord blood donation process is opening up new avenues for the treatment of neurological disorders such as cerebral palsy and autism. Studies have shown that cord blood stem cells can reduce inflammation and promote the repair of damaged brain tissue, potentially improving cognitive and motor functions in affected individuals.
- Autoimmune Diseases: The immunomodulatory properties of cord blood stem cells have sparked interest in their potential application for autoimmune diseases, such as multiple sclerosis and type 1 diabetes. The cord blood donation process may yield stem cells that can regulate the immune system’s response, potentially reducing inflammation and preventing further damage to the patient’s tissues and organs.
- Cardiac Repair: The cord blood donation process has led to groundbreaking research in regenerative medicine, particularly in the area of heart disease. Preclinical studies have shown that cord blood stem cells can stimulate the growth of new blood vessels and promote the repair of damaged heart tissue, offering hope for patients with heart failure and other cardiac conditions.
- Wound Healing: The cord blood donation process may also contribute to advances in wound healing and tissue regeneration. Research has demonstrated that cord blood stem cells can promote the formation of new blood vessels and stimulate the production of growth factors, accelerating the healing process in various injury models.
- Organ Regeneration: The cord blood donation process is propelling research into organ regeneration and transplantation. By differentiating cord blood stem cells into various cell types, scientists are exploring the possibility of generating functional tissues and organs that could be used for transplantation, potentially reducing the reliance on organ donors and addressing the critical shortage of organs available for transplantation.
The cord blood donation process is driving the expansion of therapeutic applications for cord blood stem cells, paving the way for new and innovative treatments across a wide range of medical conditions. As researchers continue to uncover the full potential of these remarkable cells, the cord blood donation process will play a crucial role in shaping the future of regenerative medicine and offering hope to millions of patients worldwide.
Summary
The Cord Blood Donation Process: A Lifesaving Gift with Boundless Potential
In summary, the cord blood donation process is a remarkable medical advancement that offers hope to countless patients suffering from life-threatening diseases and conditions. This vital process has already demonstrated its therapeutic value in the treatment of various blood disorders and is rapidly expanding its applications in regenerative medicine and beyond. As research continues to unlock the full potential of cord blood stem cells, the cord blood donation process stands as a testament to the power of medical innovation and the life-changing impact of selfless giving.
The cord blood donation process begins with the collection of umbilical cord blood following the birth of a healthy baby. Rich in hematopoietic stem cells, cord blood has unique characteristics that make it an invaluable resource for transplantation and other therapeutic applications. The cord blood donation process can save lives by providing a source of compatible stem cells for patients with blood-related disorders, including leukemia, lymphoma, and various inherited blood diseases.
In addition to its established role in treating blood disorders, the cord blood donation process is driving groundbreaking research in regenerative medicine. Studies are investigating the potential of cord blood stem cells to repair damaged tissue, reduce inflammation, and stimulate the growth of new blood vessels. The cord blood donation process is opening up new possibilities for the treatment of neurological disorders, autoimmune diseases, heart disease, and more, offering hope to patients with previously untreatable conditions.
The cord blood donation process also plays a crucial role in ensuring that high-quality cord blood units are available for transplantation. Public and private cord blood banks offer different options for the storage and use of cord blood, with public banks providing free storage for use by any patient in need, while private banks store cord blood exclusively for the donor’s family. Both options have their benefits and limitations, and the choice ultimately depends on the individual’s priorities and financial considerations.
Ensuring the safety and quality of cord blood units is paramount to the success of the cord blood donation process. Accreditation by organizations such as AABB and FACT, as well as adherence to FDA regulations, helps maintain high standards for cord blood banking and transplantation. These safeguards protect the health of both donors and recipients and promote confidence in the cord blood donation process.
As the cord blood donation process continues to evolve, ethical considerations surrounding informed consent, ownership, access, privacy, and confidentiality must be addressed to ensure the responsible and equitable use of this valuable resource. By fostering transparency and promoting ethical practices, the cord blood donation process can continue to thrive and improve the lives of patients worldwide.
In conclusion, the cord blood donation process is a transformative medical breakthrough with the potential to revolutionize the treatment of various diseases and conditions. By understanding the process, its benefits, and its limitations, individuals can make informed decisions about cord blood donation and contribute to a brighter, healthier future for countless patients in need.
Importance of Cord Blood Donation
The cord blood donation process is a vital medical advancement with the potential to save lives and improve the quality of life for countless individuals worldwide. As a rich source of hematopoietic stem cells, cord blood has unique properties that make it a valuable resource for transplantation and an essential tool in the treatment of various life-threatening diseases. The importance of the cord blood donation process cannot be overstated, as it offers hope to patients and their families, fuels groundbreaking research, and contributes to the development of innovative therapies.
One of the key reasons the cord blood donation process is so important is its ability to provide a lifesaving treatment option for patients with blood-related disorders. The stem cells found in cord blood can be used to treat a wide range of conditions, including leukemia, lymphoma, and inherited blood diseases such as sickle cell anemia and thalassemia. For many patients, a cord blood transplant may be their best chance for a cure or long-term remission.
The cord blood donation process also has a significant advantage over traditional bone marrow donation, as it offers greater flexibility in terms of donor compatibility. Cord blood stem cells have a lower risk of graft-versus-host disease (GVHD), a serious complication that can occur following a stem cell transplant. This lower risk allows for a broader range of potential donor-recipient matches, increasing the likelihood that patients will find a suitable donor.
Another crucial aspect of the cord blood donation process is its role in advancing medical research. The unique properties of cord blood stem cells have generated significant interest among scientists and researchers, who are exploring their potential in regenerative medicine, gene therapy, and other cutting-edge fields. By donating cord blood, individuals are not only providing a valuable resource for patients in need but also contributing to the development of new treatments and therapies that could benefit countless others in the future.
In addition to the direct benefits for patients and research, the cord blood donation process has broader implications for public health and healthcare systems. The availability of cord blood for transplantation can help to reduce healthcare costs, as patients who receive successful transplants often require fewer long-term medical interventions and hospitalizations. Furthermore, the cord blood donation process can help to address disparities in access to transplantation, particularly for patients from underrepresented ethnic and racial groups, who often face challenges in finding suitable donors.
Finally, the cord blood donation process is an opportunity for expectant parents to make a meaningful, lasting impact on the lives of others. By choosing to donate their baby’s cord blood, they are giving a priceless gift of hope to patients and their families, as well as contributing to the advancement of medical science. The cord blood donation process is a powerful reminder of the potential for individual actions to make a profound difference in the world.
The importance of the cord blood donation process cannot be overstated. Its potential to save lives, drive medical innovation, and promote health equity make it a critical component of modern healthcare. By raising awareness and encouraging more individuals to participate in the cord blood donation process, we can help to unlock the full potential of this remarkable resource and transform the lives of countless patients in need.
Steps in the Donation Process
The cord blood donation process is a straightforward procedure that allows expectant parents to make a potentially lifesaving contribution to patients in need of a stem cell transplant. By understanding the key steps involved in the cord blood donation process, parents can make an informed decision about whether this option is right for them and their baby. This section will outline the main stages in the cord blood donation process, from initial research to the actual collection and storage of the cord blood.
Research and Education: The first step in the cord blood donation process is to become well-informed about the benefits and potential uses of cord blood, as well as the various options for donation and storage. Expectant parents should consult with their healthcare provider and research reputable sources to gain a comprehensive understanding of the cord blood donation process.
Choosing a Cord Blood Bank: Next, parents need to decide whether they want to donate to a public cord blood bank or store the cord blood privately. Public banks accept cord blood donations for use by patients in need, while private banks store the cord blood for potential future use by the donor’s family. Factors such as cost, storage policies, and accreditation should be considered when making this decision.
Registration and Consent: Once a cord blood bank has been chosen, parents must register and provide informed consent for the cord blood donation process. This involves completing necessary paperwork and discussing the procedure with their healthcare provider. Informed consent ensures that parents understand the risks and benefits associated with the cord blood donation process, as well as their rights and responsibilities.
Prenatal Planning: As part of the cord blood donation process, expectant parents should inform their healthcare provider of their decision to donate cord blood. This allows the provider to make necessary arrangements and ensure that the cord blood collection kit is available at the time of delivery.
Delivery and Cord Blood Collection: The actual cord blood donation process takes place immediately after the baby’s birth. The healthcare provider will collect the cord blood by clamping and cutting the umbilical cord, then using a needle and syringe or gravity bag to extract the blood from the cord. This process is quick, painless, and does not pose any risk to the mother or baby.
Transportation and Processing: Following collection, the cord blood is packaged and transported to the chosen cord blood bank. At the bank, the cord blood will be processed to separate the stem cells from other components, such as plasma and red blood cells. The stem cells are then cryopreserved and stored for potential future use.
Record-keeping and Follow-up: After the cord blood donation process, the cord blood bank will provide the donor with a unique identification number for their cord blood unit. Parents should keep this information for future reference, as it may be needed if the cord blood is ever required for a transplant or other medical purpose.
The cord blood donation process involves several key steps, from initial research and decision-making to the actual collection and storage of the cord blood. By understanding these stages, expectant parents can make an informed choice about whether to participate in the cord blood donation process and potentially make a significant impact on the lives of patients in need.
Future Developments and Applications
The cord blood donation process has already demonstrated significant potential for treating various life-threatening diseases and conditions. As scientific knowledge and technology continue to advance, it is likely that the scope of cord blood applications will expand, leading to even more breakthroughs in the field of regenerative medicine. This section will explore some of the most promising future developments and applications related to the cord blood donation process.
- Expansion of Cord Blood Transplantation Indications: Currently, cord blood transplantation is primarily used for treating hematopoietic disorders, such as leukemia, lymphoma, and certain inherited blood disorders. As research progresses, new indications for cord blood transplantation may emerge, potentially expanding the range of diseases and conditions that can be treated through the cord blood donation process.
- Enhancing Cord Blood Engraftment and Survival Rates: One of the challenges associated with cord blood transplantation is the relatively low engraftment rate and the potential for graft-versus-host disease (GVHD). Scientists are working on strategies to improve these outcomes, such as using gene editing technologies to modify cord blood cells or combining cord blood units to increase the number of stem cells available for transplantation. Success in these areas could make the cord blood donation process even more valuable for patients in need.
- Regenerative Medicine Applications: The cord blood donation process may also play a critical role in the field of regenerative medicine, which focuses on repairing or replacing damaged tissues and organs. Cord blood-derived stem cells have shown potential for treating conditions such as spinal cord injuries, heart disease, and neurological disorders like Parkinson’s disease and multiple sclerosis. As research in this area advances, the cord blood donation process could provide a valuable source of cells for regenerative therapies.
- Gene Therapy and Genome Editing: Another exciting area of research related to the cord blood donation process is gene therapy and genome editing. These technologies have the potential to correct genetic mutations that cause diseases and disorders, effectively curing patients of their condition. For example, scientists are exploring the use of cord blood-derived stem cells to treat genetic conditions like sickle cell anemia and thalassemia through gene editing techniques like CRISPR/Cas9. The success of these therapies could lead to an increased demand for cord blood donations and further expand the applications of the cord blood donation process.
- Personalized Medicine: The future of medicine is increasingly moving towards a personalized approach, in which treatments are tailored to an individual’s unique genetic makeup and medical history. Cord blood-derived stem cells may play a key role in this shift, as their unique properties and ability to differentiate into various cell types make them ideal for personalized therapies. As the field of personalized medicine continues to grow, the cord blood donation process could become an integral part of developing targeted treatments for a wide range of diseases and conditions.
- International Collaboration and Cord Blood Banking: To maximize the potential benefits of the cord blood donation process, increased international collaboration and standardization in cord blood banking practices are essential. This includes sharing best practices, improving the efficiency of cord blood banking systems, and ensuring equitable access to cord blood units for patients worldwide. By working together, the global medical community can ensure that the cord blood donation process continues to save lives and improve the quality of life for countless individuals.
The future of the cord blood donation process holds immense promise, with the potential to revolutionize the treatment of numerous diseases and conditions. As research and technology continue to advance, it is likely that the scope and impact of the cord blood donation process will only continue to grow, making it an increasingly vital resource in the fight against illness and disease.
Frequently Asked Questions (FAQs)
Is Cord Blood Donation Painful or Harmful to the Mother or Baby?
Cord blood donation is neither painful nor harmful to the mother or baby. The process of collecting cord blood occurs after the baby’s birth and after the umbilical cord has been clamped and cut, which ensures that there is no direct impact on the baby. The collection process typically takes just a few minutes and is performed by the healthcare provider or a trained cord blood collection specialist.
During the cord blood collection, the baby is not in any discomfort, as they are already separated from the umbilical cord. The process does not interfere with the immediate care of the newborn, such as skin-to-skin contact or initial breastfeeding. Furthermore, since the umbilical cord has no nerve endings, the process is painless for both the baby and the mother.
For the mother, there is no additional pain or discomfort associated with cord blood donation. The collection process takes place after the delivery of the baby and the placenta, so it does not interfere with the birthing process or cause any additional complications. In fact, many mothers may not even be aware that the cord blood is being collected, as they are focused on their newborn and recovering from the delivery.
Cord blood donation is a safe and painless procedure for both the mother and the baby. The benefits of cord blood donation, such as providing a valuable source of stem cells for transplantation and potential regenerative medicine applications, far outweigh any minimal risks associated with the collection process.
Can I Donate Cord Blood if I Have a Family History of Certain Diseases?
Yes, you can still donate cord blood even if you have a family history of certain diseases. However, eligibility criteria for cord blood donation may vary depending on the cord blood bank or donation program you choose. It’s important to contact your chosen cord blood bank or donation program directly to discuss your specific situation and determine if you meet their requirements.
Having a family history of certain diseases may impact the acceptance of your cord blood donation. Some diseases or genetic conditions with a strong familial component may disqualify you from donating cord blood. This is because cord blood stem cells can potentially carry genetic predispositions or markers for certain diseases that may affect the recipient if transplanted.
The specific diseases or conditions that may affect your eligibility can vary, so it’s important to have a discussion with the cord blood bank or donation program to understand their guidelines and requirements. They will assess your family history, medical history, and any other relevant factors to determine your eligibility.
It’s worth noting that even if you’re unable to donate cord blood due to a family history of certain diseases, you can still consider private cord blood banking. Private banking allows you to store your baby’s cord blood for personal use in case it’s needed for your immediate family members in the future.
How Long Can Cord Blood be Stored and Remain Viable?
Cord blood can be stored and remain viable for an extended period of time if properly processed and cryopreserved. The current scientific consensus suggests that cord blood can be stored for at least 15 to 20 years while maintaining its viability and functionality. Some studies have even reported successful preservation and viability of cord blood samples for up to 23 years.
Cryopreservation, which involves freezing the cord blood at very low temperatures (-196°C or -320.8°F) using cryoprotectant solutions, is the key method used to store cord blood for long-term preservation. The freezing process halts cellular activity and preserves the integrity of the cord blood stem cells.
Cord blood banks follow strict protocols to ensure the optimal preservation of cord blood samples. These include using specialized freezing techniques, employing controlled-rate freezing, and storing the samples in well-maintained liquid nitrogen storage tanks to maintain the required ultra-low temperatures.
It’s important to note that while cord blood can remain viable for many years, the long-term storage duration may vary depending on the specific cord blood bank or storage facility. Different banks may have different protocols and storage conditions, so it’s advisable to inquire about their storage practices and policies.
Continual advances in preservation techniques and research are further improving the potential for longer storage and viability of cord blood. However, it’s always recommended to consult with a reputable cord blood bank or storage facility for the most up-to-date information on storage durations and viability.
What are the Costs Associated with Cord Blood Donation and Storage?
The costs associated with cord blood donation and storage can vary depending on several factors, including the specific cord blood bank or donation program you choose, whether you opt for public or private banking, and the services included in the package. Here’s a general overview of the potential costs involved:
Cord Blood Donation: If you choose to donate your baby’s cord blood to a public cord blood bank, typically there are no costs involved for the donor. Public banks collect and store cord blood units for public use, and the expenses are usually covered by the bank or through government funding.
Private Cord Blood Banking: Private cord blood banking involves storing your baby’s cord blood exclusively for your family’s future use. Private banking typically incurs upfront fees and ongoing storage fees. The costs can include:
Enrollment or processing fee: This is a one-time fee charged to cover the collection, testing, and processing of the cord blood unit. It can range from a few hundred to a few thousand dollars.
Annual storage fee: Private banks charge an annual fee for the ongoing storage and maintenance of the cord blood unit. The annual storage fee can range from a few hundred to a few thousand dollars.
Additional services: Some private cord blood banks offer additional services such as expanded genetic testing, medical courier fees, or insurance options. These services may have separate costs associated with them.
It’s important to thoroughly research and compare different cord blood banks or programs to understand their pricing structures, payment plans, and any additional fees they may charge.
Additionally, it’s worth noting that some private cord blood banks may offer financial assistance programs, discounts, or financing options to help make the cost of private banking more manageable for families.
Remember, the costs associated with cord blood donation and storage can vary, so it’s essential to contact the cord blood bank directly to get accurate and up-to-date information about their pricing and payment options.
Can I Access My Child’s Donated Cord Blood if Needed in the Future?
If you have donated your child’s cord blood to a public cord blood bank, it is generally not retrievable for personal use in the future. Public cord blood banks collect and store donated cord blood units for the purpose of providing them to patients in need of a stem cell transplant. Once donated, the cord blood becomes part of the public inventory and is available to any patient who matches the cord blood unit.
On the other hand, if you have chosen private cord blood banking, you can typically access and use the stored cord blood for your child or other eligible family members if needed in the future. Private cord blood banks store the cord blood unit exclusively for your family’s use. It can be retrieved from storage if there is a medical need that can be addressed using the stem cells present in the cord blood.
Private cord blood banks have specific protocols in place to facilitate the retrieval process when needed. It’s important to familiarize yourself with the policies and procedures of your chosen private cord blood bank regarding the retrieval and release of stored cord blood units.
It’s worth noting that the decision to privately bank cord blood is a personal one, and the potential benefits and limitations should be carefully considered. Discussing the option with your healthcare provider can provide further guidance based on your specific circumstances and medical history.



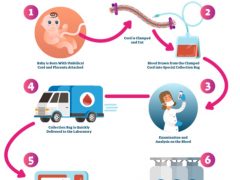





Great post. I was checking constantly this blog and I’m impressed!
Very useful info particularly the last part :
) I care for such information a lot. I was looking for this certain information for a long time.
Thank you and best of luck.
If you are going for finest contents like I do, simply visit this site daily for
the reason that it presents feature contents, thanks
hey there and thank you for your info – I have definitely picked up anything
new from right here. I did however expertise a few technical points using this web site, as I experienced to reload the web site many times previous
to I could get it to load correctly. I had been wondering if your
hosting is OK? Not that I’m complaining, but sluggish loading instances times will
very frequently affect your placement in google and could damage
your high quality score if ads and marketing with Adwords.
Well I am adding this RSS to my email and could look out for much more of your respective intriguing
content. Make sure you update this again soon.
Howdy very nice site!! Guy .. Beautiful .. Superb ..
I will bookmark your blog and take the feeds additionally?
I am happy to seek out numerous helpful info here within the post,
we want develop extra strategies in this regard, thanks
for sharing. . . . . .
This post provides clear idea in support of the
new users of blogging, that in fact how to do blogging
and site-building.
《539彩券:台灣的小確幸》
哎呀,說到台灣的彩券遊戲,你怎麼可能不知道539彩券呢?每次”539開獎”,都有那麼多人緊張地盯著螢幕,心想:「這次會不會輪到我?」。
### 539彩券,那是什麼來頭?
嘿,539彩券可不是昨天才有的新鮮事,它在台灣已經陪伴了我們好多年了。簡單的玩法,小小的投注,卻有著不小的期待,難怪它這麼受歡迎。
### 539開獎,是場視覺盛宴!
每次”539開獎”,都像是一場小型的節目。專業的主持人、明亮的燈光,還有那台專業的抽獎機器,每次都帶給我們不小的刺激。
### 跟我一起玩539?
想玩539?超簡單!走到街上,找個彩券行,選五個你喜歡的號碼,買下來就對了。當然,現在科技這麼發達,坐在家裡也能買,多方便!
### 539開獎,那刺激的感覺!
每次”539開獎”,真的是讓人既期待又緊張。想像一下,如果這次中了,是不是可以去吃那家一直想去但又覺得太貴的餐廳?
### 最後說兩句
539彩券,真的是個小確幸。但嘿,玩彩券也要有度,別太沉迷哦!希望每次”539開獎”,都能帶給你一點點的驚喜和快樂。
Hey I know this is off topic but I was wondering if you knew of any
widgets I could add to my blog that automatically tweet my
newest twitter updates. I’ve been looking for a plug-in like this for
quite some time and was hoping maybe you would have some experience with something like this.
Please let me know if you run into anything. I truly enjoy reading your blog and I look forward to your new updates.
I am sure this post has touched all the internet users,
its really really fastidious paragraph on building up
new web site.
order azithromycin 500mg online
reliable canadian pharmacy
synthroid 12.5 mg
metformin online buy
tadalafil pills canada
discount tadalafil
order prednisone online no prescription
tadalafil tablets 2.5mg india
pharmacy express
buying prednisone mexico
zyprexa im
order valtrex online uk
cialis 5mg price canada
northwestpharmacy
azithromycin 1200 mg daily
glucophage 100 mg
big pharmacy online
where to buy metformin
super saver pharmacy
pharmacy rx
metformin 1mg